Weekly Checkup
November 10, 2022
For Those Who Have Borne the Battle
On this Veterans Day, I’d like to review one way in which we try to repay those who gave so much of themselves to this nation. The ethos of our veterans’ health care system goes all the way back to President Lincoln’s Gettysburg Address: “. . . let us strive on to finish the work we are in, to bind up the nation’s wounds, to care for him who shall have borne the battle and for his widow, and his orphan . . . .” By 1865, Congress had established the National Home for Disabled Volunteer Soldiers. Eventually, veterans’ health services grew to become what is now called the Veterans Health Administration (VHA), housed within the Department of Veterans Affairs.
So, how is eligibility determined for VHA services? Not all former military members are eligible to receive VHA services. First and most obvious, they must meet the definition of a veteran: an “individual who served in the active military, naval, or air service and who was discharged or released under conditions other than dishonorable.” Second, they must have served a minimum of 24 months of continuous active duty, not including training. Even if veterans meet these eligibility requirements, however, they may not be allowed to enroll in VHA’s system as VHA funding is discretionary. Thus, if funds are limited, veterans who do not meet certain priority thresholds may not be enrolled in the system. Enrollment is only guaranteed if the veteran has a service-connected disability, is a former prisoner of war, was exposed to certain toxic substances and environmental hazards, or has an income that falls below a certain threshold.
Enrolled veterans receive a standard set of medical benefits. Generally, these include a broad spectrum of services, among them preventive and primary care, as well as inpatient, outpatient, surgical, and prescription drug services. Covered services also generally include durable medical equipment, home health services, hospice and palliative care, noninstitutional adult day health care, and respite services. The VHA also provides gender-specific services for women, including maternity and newborn care. Dental care services and eligibility are much narrower than standard medical care services, and aside from former prisoners of war and those with specific service-connected dental conditions, are basically only provided if a dental condition is caused by service-connected injuries or is aggravating service-connected injuries.
Do veterans have to pay for their VHA services? There are no premiums for VHA care, but if treatment is not related to a service-connected condition, there may be copayments involved depending on the veteran’s priority category and the type of care. Only those in Priority Category 1, who have been rated 50 percent or more service-connected disabled or have received the Medal of Honor, are never charged a copayment regardless of the type of care received or whether treatment is service-connected. Priority Categories 1-5 are never charged copayments for inpatient or outpatient services, with some exemptions for Priority Category 6 veterans. Priority Category 7 veterans are responsible for 20 percent of the VHA’s inpatient copayment, and Priority Category 8 veterans are responsible for the full initial copayment. Veterans, regardless of Priority Category, can never be charged more than one copayment in a day.
Our nation owes a great debt to our veterans, and this newsletter does not have nearly enough space to cover the deficiencies in VHA services and the many difficulties that veterans face when trying to receive care. What this newsletter can do is urge policymakers of all stripes to ensure that those who have borne the battle receive our nation’s full measure of devotion in providing the care these veterans have so rightly earned.
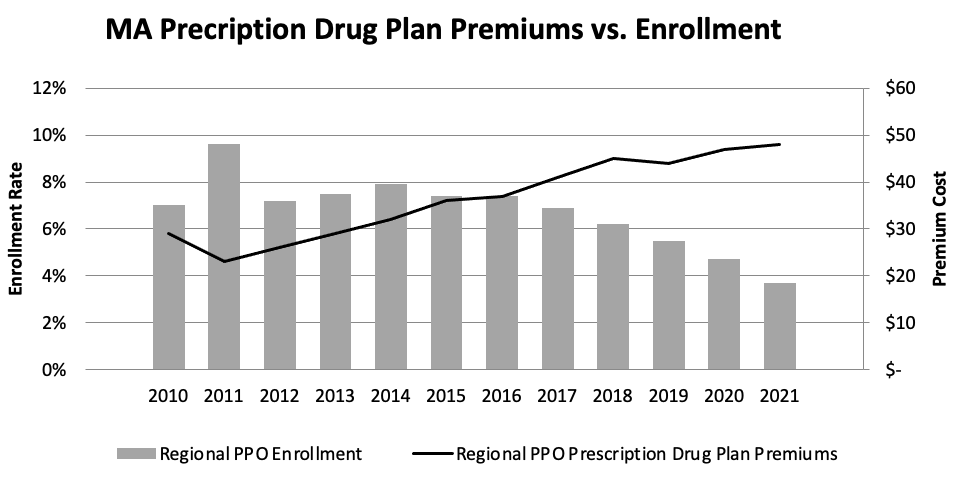
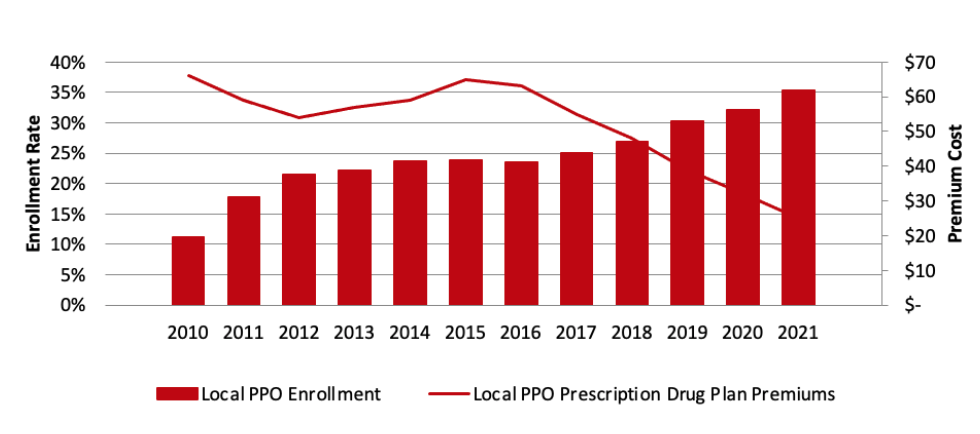
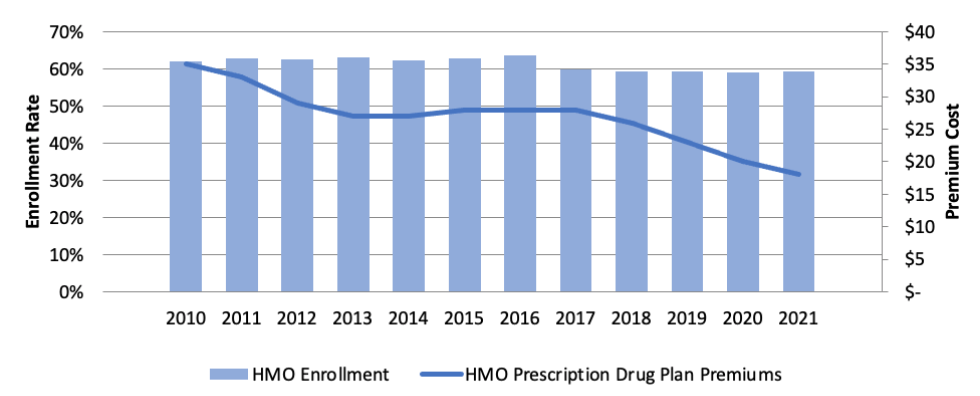
Chart Review: Comparison of Medicare Advantage Part D Premiums and Enrollment Rates
Danielle Bartolotta, Health Care Policy Intern
There are three primary types of Medicare Advantage plans: Health Maintenance Organization (HMO), local Preferred Provider Organization (local PPO), and regional Preferred Provider Organization (regional PPO). As the charts below show, over the past five years, HMO premiums – inclusive of the Part D drug programs – and enrollment have been largely stable, while local PPOs saw premium prices drop and enrollment increase. On the other hand, regional PPOs – which were created to provide individuals in medically underserved rural communities greater access to MA plans – have seen premiums increase since 2011 and enrollment decrease since 2016. The reasons for the increasing premiums in regional PPO plans are unclear. Policymakers should investigate why these plans’ premiums are increasing – driving reduced enrollment – to ensure beneficiaries continue to see improved health outcomes.
Data Sources: RUPRI Medicare Advantage Enrollment Update 2021 and KFF Medicare Advantage in 2022