Weekly Checkup
July 15, 2022
Resistance on the Rise
There will be many discussions over the next several years about what we learned from the COVID-19 pandemic and the response to it. There must also be a discussion about the things we missed when our focus was squarely on the virus itself—among them, the growing problem of antimicrobial resistance (AMR). AMR has major implications for our health care system: A new Centers for Disease Control and Prevention (CDC) report found that both infections and deaths attributed to AMR increased by 15 percent in 2020, nearly erasing the 18 percent decrease seen between 2012–2017.
As a brief reminder, AMR happens when bacteria adapt to antibiotics and evolve to a point such that they no longer respond to medicines. AMR is exacerbated by the misuse and overuse of antibiotics, accelerating the evolution of bacteria beyond our current ability to treat them. This process has disastrous consequences for humans: So-called “superbugs” threaten to wreak havoc across the globe.
What drove this massive increase in AMR-related infections and deaths? In large part, it was due to the lack of knowledge about COVID-19 and the numerous adjustments our medical system had to make to handle it in the early days of the pandemic. Between March and October of 2020, almost 80 percent of patients hospitalized because of COVID-19 were given antibiotics, likely because of how similar the virus’ symptoms appeared to those of pneumonia during initial patient assessments. Rapid tests were not widely available for much of 2020, so COVID-19 cases could not be easily and quickly identified.
Other drivers of AMR noted by CDC include overwhelmed labs and reduced testing for non-COVID infections. Bacterial submissions to the CDC’s testing lab network were down 21 percent in 2020, and some of the network labs were repurposed to test for COVID-19, leading to backups.
Hospital infection protocol also took a hit during the early days of the pandemic. Personal protective equipment (PPE) was scarce and infection protocol staff were often redirected to help COVID patients. Making things worse, hospitals faced a deluge of patients who had longer stays in the hospital requiring more frequent use of things such as catheters and ventilators, creating greater exposure to hospital-acquired infections (HAI). Of the more than 29,400 people who died from AMR infections during 2020, 40 percent were due to HAI.
Adding to all of this, the CDC states that many people with bacterial infections who otherwise would have gone to the hospital for treatment avoided doing so, allowing the infection to run its course. With mild infections, this typically isn’t a problem, but with severe infections such as tuberculosis, it can be deadly. Even if they aren’t deadly, bacterial infections can grow and mutate inside a person and spread further around a community if left untreated, potentially leading to bacteria that are harder to eradicate.
Finally, the problem of AMR could be even worse than we know: For nine of the 17 identified AMR threats, 2020 data are delayed or unavailable, meaning we don’t yet know the extent of the problem. To be clear, the growth of AMR threats—and certainly the increases in cases and deaths—is both alarming and tragic; it also would have been incredibly difficult to avoid. Doctors followed standard protocol when prescribing antibiotics to patients who presented with pneumonia-like symptoms, and hospitals faced a crush of patients so that normal protocols had to be quickly adjusted to meet current conditions. And decisions had to be made with the information available at the time—even information as sparse as what we had in the beginning of the pandemic.
Regrettably, there are no easy answers, as it is impossible to guess the exact needs of patients during the next health crisis. It is nevertheless useful to ensure we learn all we can about what went right—and what went wrong—in the response to the COVID-19 pandemic. One lesson to take from this is the importance of ensuring our health system remains flexible enough to handle a variety of challenges. The CDC suggests that this will require a more secure medical supply chain, investment in lab networks for larger capacity so they can continue testing for bacterial infections simultaneously with new diseases, and foresight of public health officials, hospitals, and providers to continue to account for collateral events during large health emergencies. That’s a difficult challenge, but with the next health crisis always around the corner, it’s one we must face.
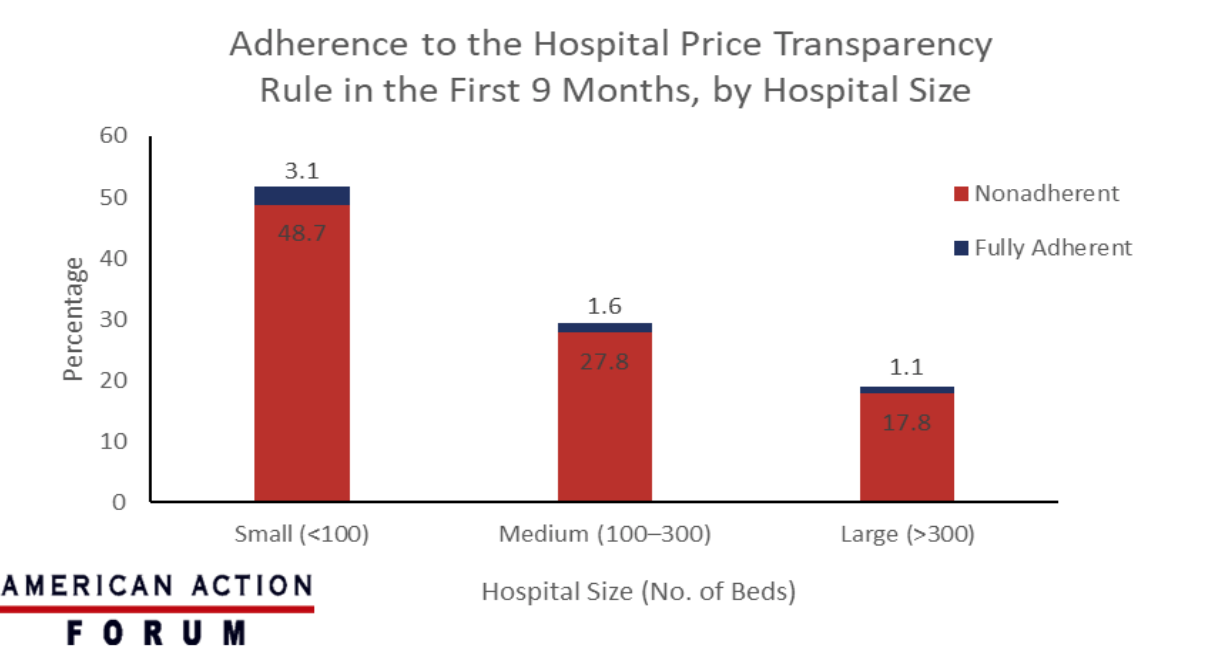
Chart Review: Hospital Adherence to Price Transparency Final Rule
Evan Turkowsky, Health Care Policy Intern
On July 1, the Transparency in Coverage Final Rule issued by the Centers for Medicare and Medicaid Services (CMS), which requires health insurers to publish prices paid for services from hospitals and physicians, went into effect. The rule is intended to increase health care price transparency for patients. Yet initial compliance with the similar hospital price transparency final rule that required hospitals to disclose their prices starting in January 2021 offers a cautionary tale. In a recent report from the Journal of the American Medical Association (JAMA) Network, researchers found that only 5.7 percent of the 5,239 hospitals registered with CMS adhered to the hospital price transparency final rule in the first nine months. As seen in the chart below, the majority of assessed hospitals (51.8 percent) were classified as small—those containing fewer than 100 beds—and only 3.1 percent initially adhered to the transparency rule. Similarly, 1.6 percent of assessed hospitals were classified as medium and fully adherent with the rule within the first nine months and 1.1 percent were large and fully adherent. The main reasons for nonadherence included no shoppable display and/or no machine-readable files. According to a report from PatientRightsAdvocate.org, only 14.3 percent of all hospitals had fully adhered to the rule after the first 12 months.
Data Source: The JAMA Network and PatientRightsAdvocate.org