Weekly Checkup
June 10, 2022
340B Gets Its Day in Court
Unless you’ve been under a rock, you’re probably aware that the Supreme Court has a lot going on right now. With the upcoming Dobbs v. Jackson Women’s Health Organization abortion-rights decision dominating the news, you may have missed a big drug pricing ruling that’s due any day: the decision in American Hospital Association (AHA) v. Becerra will determine just how much the administration can do to make changes to the broken 340B Drug Pricing Program (340B).
To start, here’s a brief background on 340B: In 1990, Congress created the Medicaid Drug Rebate Program (MDRP), which, among other things, legally required drug manufacturers to give Medicaid the “best price” of any purchaser. Before this, pharmaceutical companies had a history of discounting or donating medicines to hospitals for charity care in return for tax breaks and community goodwill. But as the best price rule in MDRP did not exclude charitable donations, Medicaid would be getting drugs for free if the donations continued, naturally causing the discounts and donations to dry up quickly. In response to this unintended consequence, Congress created the 340B Program in 1992, whereby drug manufacturers would be required to give covered entities (CEs) – those hospitals and medical clinics who met the criteria necessary to join the 340B Program – a discount on any drugs that manufacturer wanted included in Medicaid and Medicare’s formularies. CEs will then be reimbursed by private payers and insurers at standard rates, providing CEs with a net profit on the 340B drugs that CEs are supposed to use to provide more patients with more care. Given that 340B hospitals conduct less charity care than non-340B hospitals, it is questionable whether indigent patients are benefiting from this program. More details on the program can be found in this AAF primer, and a more in-depth explanation of the problems inherent in 340B can be found in this AAF primer.
As for AHA v. Becerra, the case revolves around a 2018 rule implemented by the Trump Administration that in essence would cut drug reimbursements to 340B hospitals to more accurately reflect the 340B discount the hospital received in purchasing the drug. The rule would have changed the formula for Medicare Part B drug reimbursements to 340B hospitals from Average Sales Price (ASP) plus 6 percent to ASP minus 22.5 percent. This would be an almost 30-percent reduction in total reimbursement, which is significant for a program that was worth over $38 billion to hospitals in 2021. Naturally, the hospitals have sued to stop this rule, claiming the Department of Health and Human Services (HHS) did not have the statutory authority to make this change. But HHS is given deference in statute to update payments to represent actual costs to providers – if it has accumulated the necessary amount of cost-survey data to support that change. The AHA insists that because HHS does not have sufficient cost-survey data to support the change, it has not met the standard for Chevron Deference. A discussion of that legal test is beyond the scope of this analyst’s expertise, but suffice it to say that this court case is a very big deal for the health care system and a notable test of an important legal precedent.
Regrettably, this case also highlights yet another failure of Congress to act. The 340B Program has been in need of reform for years, but the last legislative adjustment—via the Affordable Care Act in 2014—simply expanded both 340B and its problems. Predictably, when Congress fails to fix a problem, the administrative state is ready at the wings to step in. To prevent the inherent instability involved in executive rulemaking and provide some predictability for the health care system, Congress should consider reforms to 340B before the president or the courts do.
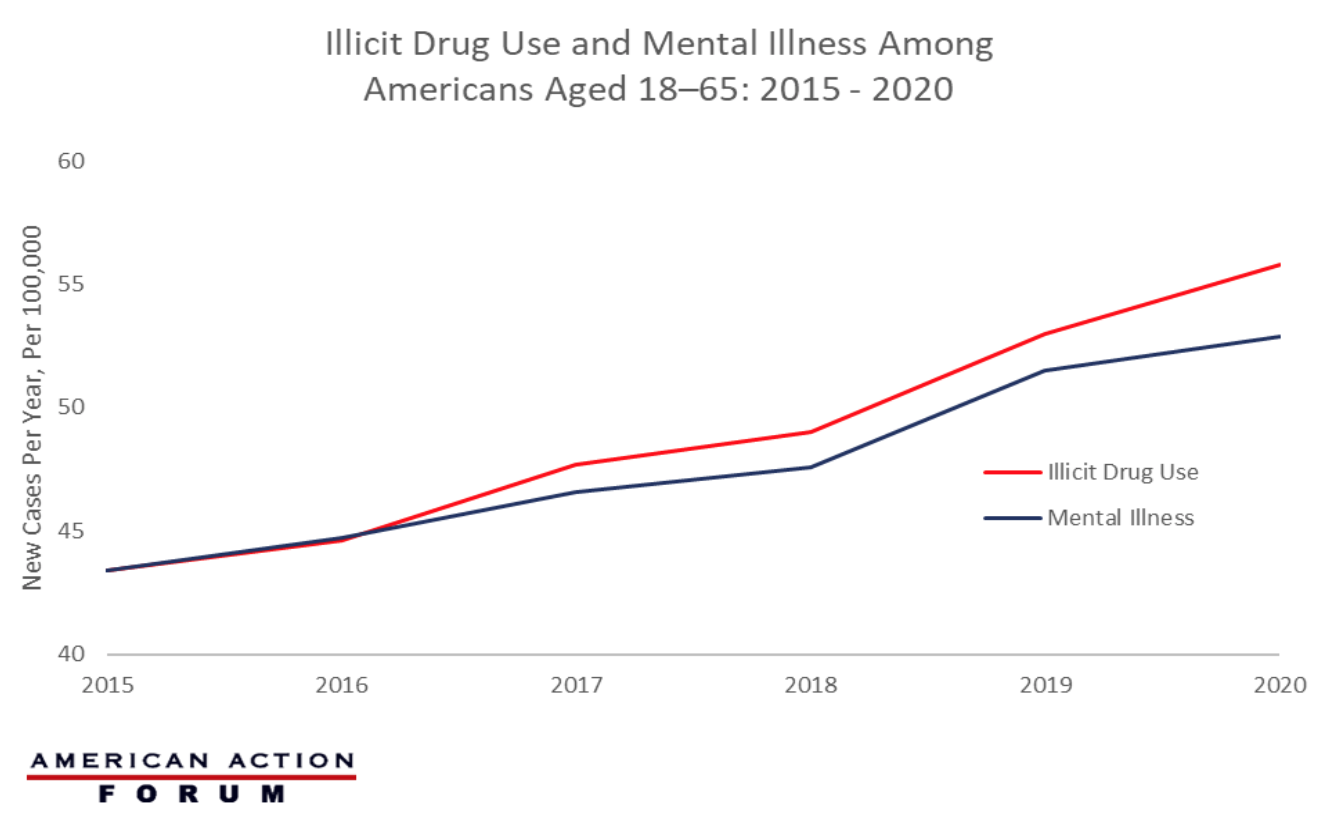
Chart Review: Illicit Drug Use and Mental Illness
Evan Turkowsky, Health Care Policy Intern
In July of this year, the Federal Communications Commission will begin rolling out the nationwide “988” phone number—an emergency hotline for the growing number of Americans suffering with mental illness that, like 911, provides an easy-to-remember number to access suicide prevention and mental health crisis counselors. Mental illness and substance use disorders affect nearly 64.5 million adults between the ages of 18 and 65 and more than 25 percent of adults who have a serious mental illness also have a co–occurring substance use disorder. As the graph below shows, the number of Americans who are diagnosed with a mental illness and those who have an onset of illicit drug use have simultaneously increased since 2015. From 2015–2020 (the last year for which there are comprehensive data), there have been over 9.5 million mental illness diagnoses and more than 9 million Americans turning to illicit drug use. In 2015, the rates of new illicit drug use and onset of mental illness were both around 43.4 cases per 100,000, while in 2020, these rates climbed to 55.8 per 100,000 and 52.9 per 100,000, respectively.