Weekly Checkup
October 6, 2023
340B Under the Microscope
The 340B Drug Pricing Program always seems to find itself in the news, which is handy because the American Action Forum’s health team will never get tired of talking about it. At the end of last week, Ranking Member of the Senate Health, Education, Labor, and Pensions Committee Senator Bill Cassidy (R-LA) announced an investigation into hospital revenue generated by the 340B Program, specifically focusing on Richmond Community Hospital (RCH) and the Cleveland Clinic. Let’s discuss the investigation and what issues Sen. Cassidy intends to explore.As regular readers will recall, Congress intended for the 340B Program to “stretch scare federal resources as far as possible, reaching more eligible patients and providing more comprehensive services.” In theory, the program does this by requiring pharmaceutical manufacturers that participate in Medicaid (itself a requirement of participating in Medicare) to provide qualifying covered entities (CEs) with large discounts on drugs. Those CEs can then turn around and sell those drugs at a higher price, and use the profits to, in theory, “provid[e] more comprehensive services” to more eligible patients. In practice, it has been found that 340B-eligible hospitals offer less charity care than the national average: The average percentage of charity care compared to patient revenues for all hospitals in 2017 was 2.03 percent, while the average percentage of charity care for 340B hospitals was 1.66 percent.Concerns about the appropriate use of 340B funds are precisely why Sen. Cassidy is investigating RCH and the Cleveland Clinic. Sen. Cassidy sent both hospitals a letter outlining his concerns and asking several questions of each. Last year, RCH was the subject of a lengthy New York Times investigation that uncovered several concerning practices. The investigation discovered that RCH had generated $90 million in profits in 2021, with a “vast majority” of its profits coming from the 340B Program. RCH’s parent company, Bon Secours, reduced core services at RCH, while expanding off-campus outpatient clinics (which still receive the 340B discount through their relationship to the CE) into wealthier suburban communities. According to the Hospital Cost Tool produced by the National Academy for State Health Policy, RCH spent 1.3 percent of its net patient revenues on charity care.The Cleveland Clinic’s 340B practices have also raised questions. A newcomer to the 340B Program in 2021 (due to a recent classification as a “rural referral center” despite being in the heart of Cleveland), the Cleveland Clinic’s flagship hospital generated $1.35 billion in net income in 2021, with approximately $136 million in revenue from the 340B Program. Ranked as the second-best hospital on the planet, the Cleveland Clinic’s charity care contributions amounted to 0.69 percent of net patient revenue. Sen. Cassidy also raised concerns about consolidation by hospitals, which may be incentivized to buy up more physician practices in order to have more off-campus outpatient clinics and thus more opportunities for 340B dollars.Both letters to both hospitals contained a series of relevant questions: Do these hospitals pass along all 340B savings to patients? If not, how much of the savings do patients see? What was the total dollar amount generated by the 340B Program, broken down by site of service? How much 340B money went toward capital improvement, executive compensation, or off-campus outpatient clinics? Were provider incentives related to the 340B Program ever discussed? These questions get at the heart of the problems in the 340B Program: a lack of transparency and potential abuse of the money generated. Of course, focusing on just two hospitals is not enough. Policymakers will ultimately need to define the program’s purpose in legislation in order to make certain that funds are being used as intended.
Chart Review: Maternal Mortality and Female Opioid Deaths
Daphne Edmond, Health Care Policy Intern
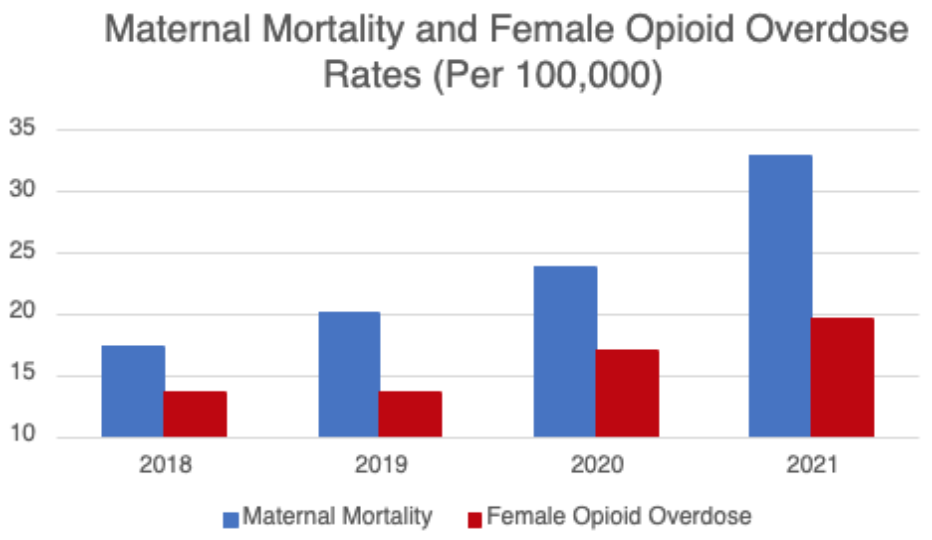
The rate of U.S. maternal death remains concerningly high compared to other similarly situated high-income nations. This high rate of maternal mortality deaths coincides with a notable increase in substance use-related deaths in women during the postpartum period, as recorded by the Centers for Medicare and Medicaid Services. The chart below demonstrates a correlation between general female opioid overdose death rates and maternal mortality rates between 2018 and 2021. Female opioid overdoses have increased substantially, with annual overdose deaths surging from 22,426 in 2018 to 32,398 in 2021 according to the National Institutes of Health. Between 2020 and 2021 there was a sizable increase in maternal mortality rates according to the Centers for Disease Control, which correlates with the increase in overdose deaths; however, female opioid overdose deaths alone do not fully account for the recent jump in maternal mortality, which may be attributed to a variety of other factors. While the maternal death rate directly attributed to drug overdose remains lower than the rate among women of childbearing age generally, it sadly remains a leading cause of maternal death.