Weekly Checkup
August 14, 2020
The Harris Pick and Health Policy
Former Vice President Joe Biden paved his path to the Democratic nomination in part by setting a moderate course on health care policy, at least by comparison to other candidates. In selecting Senator Kamala Harris for his running mate, however, Biden is bringing into his potential administration a far more progressive governing partner, one who has (at least from time to time) endorsed single-payer health care and the end of private health insurance. So, what does the Harris pick mean for health policy in a hypothetical Biden Administration?
The first thing to note is that neither Biden nor Harris have been leaders on health policy. While Biden may have tacked moderate during the campaign, Harris’s erratic back and forth on health policy was likely a major factor in her exit from the race before a single vote had been cast. For example, she cosponsored Senator Sanders’ single-payer health care legislation and has claimed to both support and oppose the elimination of private insurance at various points. While still a candidate for president, she released an all-of-the-above proposal for health care reform where she namechecked nearly every Democratic idea for health reform short of single-payer, but sort of endorsed that as well. The Harris proposal included public options, Medicare Buy-In, and some sort of “Medicare Transition Plan” into which various categories of Americans would be automatically enrolled. At the end of 10 years—yes, 10 years—the Harris proposal would lead to Medicare for All, unless of course you want private insurance, in which case there maybe, possibly, could be some form of private insurance, because she supports single-payer, but also doesn’t support ending private insurance.
Harris’s vacillation indicates a desire to match the mood of the Democratic party. Similarly, Biden’s approach to at least appear moderate makes sense electorally for two reasons. First, most Americans don’t support single-payer insurance when it’s explained to them. Second, claiming the legacy of the Affordable Care Act (ACA) helps Biden make the case that his administration would be a continuation of Obama’s. I have previously argued that his proposals are hardly moderate and would erode employer-sponsored insurance (ESI), driving more Americans into government-sponsored insurance while also removing constraints on ACA spending and resulting in higher health care costs. But the appearance of moderation ultimately served him well in the primary and could serve him well in the general election, as well.
The reality is that both Biden and Harris have sought throughout their careers to place themselves in the mainstream of the Democratic electorate, which means both of them have changed positions on health care multiple times. To the degree that Harris appears more progressive than Biden, it’s likely just a reflection of her shorter tenure in electoral politics as well as the politics of deep blue California. Because neither seems to have deeply held convictions about health care policy, Harris’s addition to the ticket doesn’t shift the calculus on health care in a Biden Administration.
At the same time, Harris’s demonstrated willingness to move to meet the Democratic base, paired with Biden’s similar disposition, should be cause for concern for anyone who opposes a government takeover of health care. Biden-Harris might not lead the charge on progressive health reforms, but they would willingly go along for the ride.
Chart Review: The Rise and Decline of Telehealth in Urban Areas
Lauren Simonides, Health Care Policy Intern
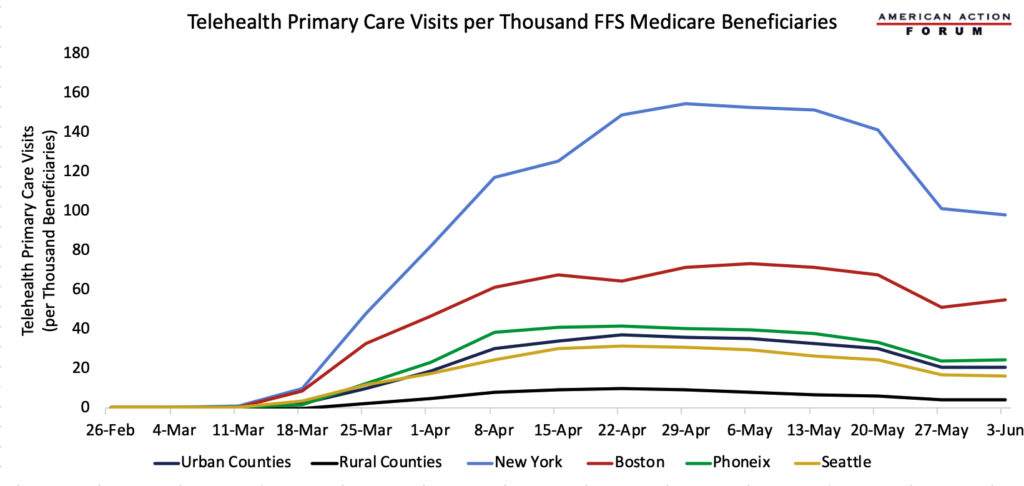
While the use of telehealth and similar technologies in health care was increasing before the COVID-19 pandemic, these technologies had mostly been reserved for more remote geographical areas. Because of the global pandemic, however, the use of telehealth throughout the United States has vastly expanded. Aggregated data from the Epic Health Research Network shows that, while comparing the number of telehealth visits from March 15, 2019, to April 14, 2019, with the number of visits during the same period in 2020, telehealth visits have increased 300-fold, consistent across age groups. Further, data from the Department of Health and Human Services, illustrated below, demonstrates that urban areas are using telehealth in record numbers as well, even more so than rural areas. As cities began to shut down, telehealth usage surged, peaking from the end of April to the end of May. The chart below indicates, however, that these numbers are beginning to drop as states began to loosen their restrictions and quarantine fatigue set in. Nevertheless, telehealth usage will likely not drop to pre-COVID-19 numbers. A survey from McKinsey and Company found that 76 percent of survey respondents said they are likely or highly likely to use telehealth moving forward. Of these respondents, only 11 percent had used telehealth in 2019. On the provider side, 57 percent of providers view telehealth more favorably than they did before COVID-19 and 64 percent are more comfortable using it.
Data from the Department of Health and Human Services
Worth a Look
Washington Post: These are the top coronavirus vaccines to watch
Health Affairs: COVID-19 Has Increased Medicaid Enrollment, But Short-Term Enrollment Changes Are Unrelated To Job Losses