Insight
June 13, 2023
Competition Takes Center Stage in Health Care Debate
Introduction
- President Biden’s executive order on Promoting Competition in the American Economy focused, in part, on hospital consolidation and its effect on health care costs and access to services.
- Several bills have been introduced, or reintroduced, in Congress, often with bipartisan support, that would fill antitrust enforcement gaps, eliminate barriers to entry, and remove an antitrust exemption for a critical residency program facilitator.
- Promoting competition and ensuring the antitrust agencies have authority to act when necessary are preconditions for reducing costs and improving care quality.
Introduction
In July 2021, President Biden issued an executive order on Promoting Competition in the American Economy. The order focused, in part, on the effects of hospital consolidation on health care costs and access to services.
Recently, Congress and executive agencies have launched investigations into pharmacy benefit managers, insurance companies, and other health care market participants as part of the broader discussion surrounding the rising costs of, and access to, health care services. Competition and antitrust enforcement in the hospital sector has taken center stage in this debate.
Several bills have been introduced, or reintroduced, in Congress that would fill the antitrust agencies’ enforcement gaps, reduce barriers to hospital entry, and remove an antitrust exemption on a critical residency program facilitator. The cumulative effect of these pieces of legislation will promote a more competitive hospital sector, which will reduce the cost of care and improve care quality and access.
Proposed Legislation
Combatting Hospital Monopolies Act
Community hospitals in the United States are a mix of for-profit hospitals, hospitals operated by state and local governments, and nonprofit hospitals. Nonprofits represent 58 percent of all community hospitals (Figure 1). There are few operational differences between nonprofit hospitals and their for-profit counterparts, but there is a noticeable difference in terms of federal oversight. Hospitals accused of engaging in activity harmful to competition are not treated equally.
Figure 1
*Graph created using data from American Hospital Association
In most other sectors of the economy, the Federal Trade Commission (FTC) would rely on the authority granted in Section 5 of the FTC Act that prohibits “unfair methods of competition…and unfair or deceptive acts or practices.” A gap in the relevant statute bars the FTC from asserting this authority to nonprofit hospitals, however.
The current statute extends the enforcement power of the agency to “persons, partnerships, or corporations” (entities regulated by other agencies or statutes are also excluded). There is a loophole: Nonprofit entities are excluded.
Representatives Pramila Jayapal (D-WA) and Victoria Spartz (R-IN) reintroduced the Combatting Hospital Monopolies Act in April 2023 to rectify this gap. The proposed legislation would amend the FTC Act by expanding the definition of corporations to include “any hospital organization or cooperative hospital service organization that is described in section 501(c)(3) of the Internal Revenue Code of 1986 and exempt from taxation under section 501(a) of such Code.”
State action, a legal doctrine, would still protect some government hospitals from federal antitrust scrutiny.
Expanding the FTC’s ability to investigate and stop the anticompetitive behavior of nonprofit hospitals, which represent more than half of all community hospitals, would help to ensure consumers are protected from any unfair or deceptive acts or practices.
Restoring Rights of Medical Residents Act
After finishing medical school, recent graduates participate in a residency program. These programs provide soon-to-be doctors an opportunity to supplement their studies with hands-on experience. The National Resident Matching Program (NRMP), known as “The Match,” facilitates this process.
The NRMP is a nonprofit organization that provides an algorithmic matching system based on the ranked preferences of both the candidate and the residency programs. Once all applicants have been considered and matched, the pairings between resident and residency program become final and binding. In 2023, 37,425 first-year post-graduate positions were offered through the NRMP, an all-time high.
While the NRMP is an efficient tool to match labor supply with demand, there are several anticompetitive concerns. These concerns were the basis of a 2002 class action lawsuit, Jung v. AAMC, filed by a group of physicians against the Association of American Medical Colleges (AAMC).
The lawsuit alleged that The Match violated Section 1 of the Sherman Act which outlaws “every contract, combination, or conspiracy in restraint of trade.” The plaintiffs argued that “the defendants,” the administrators of medical education, and the institutions that sponsor the residency programs “have contracted, combined and conspired among themselves to ‘displace competition in the recruitment, hiring, employment and compensation of resident physicians, and to impose a scheme of restraints which have the purpose and effect of fixing, artificially depressing, standardizing and stabilizing resident physician competitions and other terms of employment.’” In other words, the lawsuit alleged that the combination of the accreditation system, the binding nature of the NRMP, and the information sharing among hospitals through the AAMC resulted in a conspiracy that stripped residents of their ability to individually negotiate terms of employment including wages and working hours.
Survey data from AAMC showed that inflation-adjusted wages for first-year residents decreased 5.7 percent in 2022 from the prior year to the lowest level since the 1993–1994 survey. Meanwhile, economy-wide real wages decreased just 1.6 percent. Since 1990, inflation-adjusted wages for residents rose just 3.3 percent compared to an increase of 14.6 percent for the economy overall. Such evidence gives credence to the lawsuit’s allegations that the information exchange and the NRMP were artificially depressing wages.
As the case moved through the courts, Congress passed the Pension Funding Equity Act of 2004. Unrelated to the rest of the act was Section 207, which granted an antitrust exemption for the NRMP and as a result, Jung v. AAMC was dismissed by the court.
The Restoring Rights of Medical Residents Act, introduced by Representative Spartz, would remove the exemption by repealing Section 207 of the Pension Funding Equity Act of 2004, which could prompt future litigation similar to Jung v. AAMC. If a future case rules in favor of the plaintiffs, the restraints imposed by The Match system that prevent residents from engaging in individual negotiations over salary and other terms of employment would be removed, putting negotiating power back in the hands of residents.
Restoring Rights of Physicians to Own Hospitals Act
Hospital consolidation was a focal point of President Biden’s executive order on Promoting Competition in the American Economy, which stated that “[h]ospital consolidation has left many areas, particularly rural communities, with inadequate or more expensive healthcare options.”
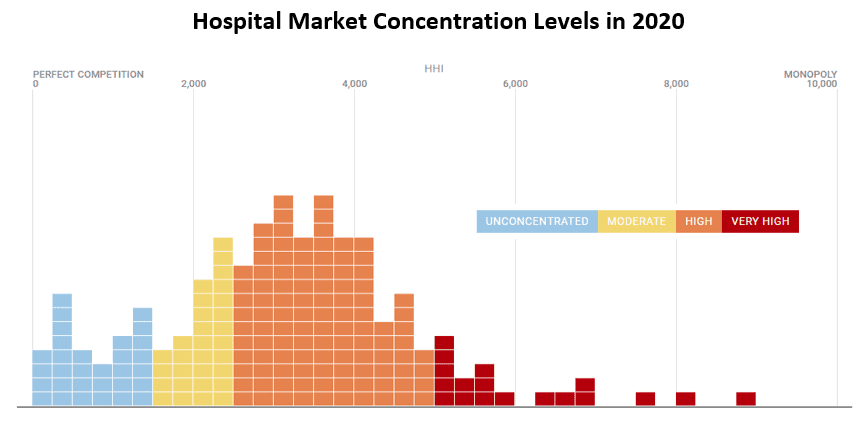
Data from the Health Care Cost Institute found that “125 metros of the 186 studied had hospital markets that were highly or very highly concentrated based on their [Herfindahl-Hirschman Index, or HHI] level.” (See Figure 2.)
Figure 2
*Data taken from Health Care Cost Institute Hospital Concentration Index
While many of these markets are considered highly or very highly concentrated, some of these markets may not be of concern to the FTC. For example, a market made up of four hospitals of equal size would have an HHI of 2,500. According to the 2010 Horizontal Merger Guidelines, 2,500 is the level dividing a market considered moderately concentrated and highly concentrated. The HHI is likely not the principal factor when the FTC determines to challenge a merger between hospitals.
To restore competition in the hospital sector, Senator James Lankford (R-OK) reintroduced the Patient Access to Higher Quality Health Care Act and Representative Michael Burgess, MD (R-TX) is leading the bill’s introduction in the House of Representatives. Additionally, Representative Spartz introduced the Restoring Rights of Physicians to Own Hospitals Act. Both bills would repeal the Affordable Care Act’s ban on “the creation and expansion of new physician-owned hospitals (POHs) and allow POHs to participate in Medicare and Medicaid.”
A white paper co-authored by Matthew Mandelberg of the Antitrust Division of the Department of Justice, Michael Smith of the Federal Trade Commission, Jesse Ehrenfeld of the American Medical Association, and Brian Miller of the Johns Hopkins University School of Medicine found that POHs “present an opportunity to inject more competition into patient/consumer markets, U.S. payor markets, and markets for physician services.” They contended that “[c]ompetition in these markets is vital for reducing costs and improving quality.” Furthermore, the authors concluded that POHs would create “greater opportunities for entrepreneurship and innovation in patient care.”
The paper also explains that permitting POHs will help reverse a decades-old trend of industry consolidation. Creating more competition for hospital services will put downward pressure on price while providing patients with more options for care. Moreover, competition for physicians and staff would increase, likely boosting wages.
Conclusion
President Biden’s executive order on Promoting Competition in the American Economy propelled hospital consolidation and competition to the forefront of the broader debate over the rising cost of health care and expanding medical services.
Several bills have been introduced, or reintroduced, in Congress, often with bipartisan support, that would fill antitrust enforcement gaps, eliminate barriers to entry, and remove an antitrust exemption on a critical residency program facilitator.
Encouraging competition by removing barriers to entry and ensuring the antitrust agencies have the proper authority to act are necessary preconditions for reducing costs and improving care quality.