Insight
September 9, 2019
Maternal Mortality in the United States
Executive Summary
- The U.S. maternal mortality rate has significantly increased from 7.2 deaths per 100,000 live births in 1987 to 16.7 deaths per 100,000 live births in 2016, and the data indicate that more than half of these deaths are preventable.
- Unnecessary cesarean sections, limited receipt of proper prenatal and postnatal care, and racial or ethnic disparities are likely contributing to soaring mortality rates.
- State maternal mortality review committees are increasingly considered necessary for collecting standardized data on pregnancy-related deaths and providing recommendations and strategies for effective interventions targeting quality and performance improvements.
Introduction
Maternal mortality, as defined by the World Health Organization (WHO), refers to “the death of a woman while pregnant or within forty-two days of termination of pregnancy, irrespective of the duration and site of the pregnancy, from any cause related to or aggravated by the pregnancy or its management but not from accidental or incidental causes.”[1] While the number of reported pregnancy-related deaths in most of the world has been declining, the maternal mortality rate (MMR) in the United States has more than doubled since 1987, from 7.2 deaths per 100,000 live births that year to a peak of 17.6 in 2014 and dropping slightly to 16.7 deaths per 100,000 live births in 2016, according to the Centers for Disease Control and Prevention (CDC).[2] Other studies reported figures as high as 23.8 in 2014.[3] These numbers indicate that the United States has one of the highest MMRs in the world.
A recent report from the CDC indicates that 60 percent of these deaths could have been prevented had the mothers better understood the importance of and been able to access more easily quality prenatal and postpartum care.[4] Further, for every maternal death, there are 84 women who suffer from a severe complication.[5] As a result, the United States is increasingly one of the most unsafe countries for women giving birth.
This overview highlights the most prominent drivers of maternal mortality in the United States and then examines several policy responses to the issue.
Why is the Maternal Mortality Rate Increasing in the United States?
The United States has one of the highest maternal mortality rates, if not the highest, in the developed world, although the data tracking these deaths are not straightforward.[6] The CDC defines pregnancy-related deaths to include deaths occurring within one year of the end of a pregnancy—significantly longer than the 42-day WHO standard noted above. Comparing the numbers under the CDC definition to the figures in other countries understandably puts the United States above every other developed country. Nevertheless, only 11.7 percent of pregnancy-related deaths in the United States occur more than 42 days after birth, which would account for roughly 2 deaths per 100,000 births, meaning the United States would still have a higher MMR than every other developed country, except Mexico and Latvia.[7]
Among 2,990 pregnancy-related deaths observed in a recent CDC study, 31 percent occurred during pregnancy, 36 percent occurred on the day of delivery or within six days post-delivery, and 33 percent occurred one week to a year postpartum.[8] As these numbers imply, a range of reasons contribute to maternal mortality in the United States.
Complications Linked to Surgical Deliveries
One in three American mothers delivers her baby via cesarean section (c-section), a 500 percent increase since the 1970s, compared with roughly one in five women worldwide.[9] A c-section is a surgical procedure to deliver a baby by creating incisions in the woman’s abdomen and uterus.[10] Providers may choose this option for their patients if the baby is demonstrating signs of potential distress, the labor is perceived to be at a stalemate, or if there are other health concerns.
One study by a doctor at Harvard found, however, that the hospital where the woman is delivering her baby is the key determinant of whether or not she will undergo a surgical delivery.[11] This finding undermines the claim that a woman’s health or the health of the baby are the primary predictors of c-sections. A 2015 study in Health Affairs corroborates this claim, finding that c-section rates in U.S. hospitals varied from 7 percent to 70 percent.[12] C-sections put women at risk for infection, postpartum hemorrhaging, blood clots, and surgical injury, and for that reason they are not recommended as the primary option over vaginal delivery.[13] A recent study found that women who had c-sections were 80 percent more likely to have complications than those who delivered vaginally, and for women aged 35 and older the risk for severe complications was nearly three times greater.[14] Improper postpartum care can exacerbate complications following surgery, and many complications left untreated can lead to death.
Chronic Conditions
The number of pregnant women with chronic health conditions such as hypertension, diabetes, and chronic heart disease is rising, and these conditions put them at higher risk for complications during their pregnancy and postpartum. A recent University of Michigan study found that there was a nearly 40 percent higher prevalence of chronic conditions (specifically those conditions which pose a particular risk for mothers and babies) among pregnant women in 2014 than in the decade prior, with the greatest increases occurring among low-income women and women living in rural areas.[15] Further, the United States seems to have much higher rates of chronic conditions than people in other developed countries: A recent study found that 60 percent of adults in the United States have a chronic condition, while the European Chronic Disease Alliance notes that roughly one-third of European adults have a chronic disease.
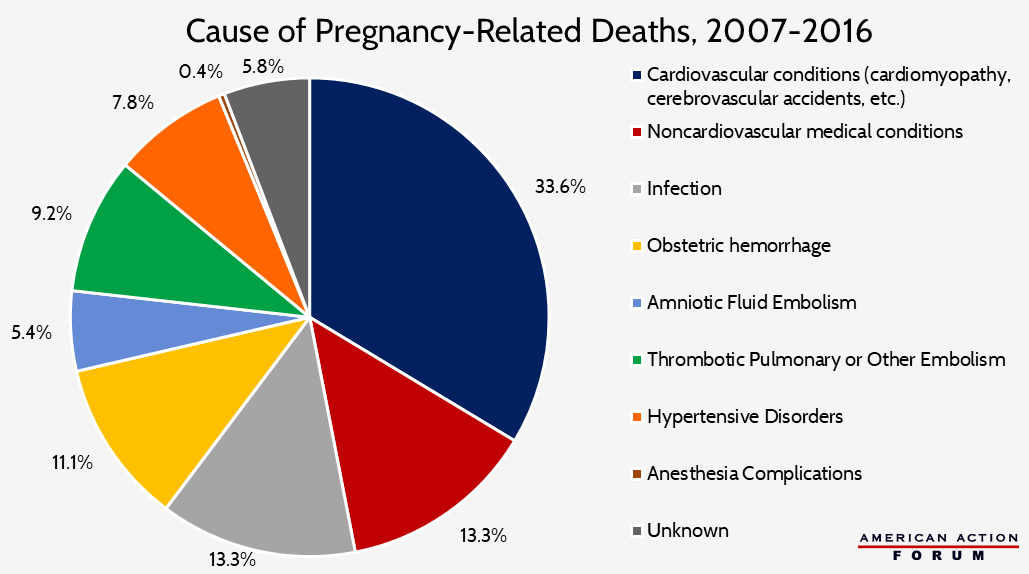
For the first time, pre-existing conditions, rather than complications with delivery, have become the leading cause of maternal morbidity and mortality.[16] Increases in cardiovascular conditions, cerebrovascular accidents (i.e. strokes), and other medical conditions were responsible for over one-third of pregnancy-related deaths from 2011 to 2015, according to CDC data. Other causes of death include hemorrhaging or amniotic fluid embolism, which were the leading causes of death at delivery. High blood pressure issues (which could be chronic or not), hemorrhaging, and infections were the most common causes of death within six days post-delivery.[17]
Source: Centers for Disease Control and Prevention. “Racial/Ethnic Disparities in Pregnancy-Related Deaths—United States, 2007-2016.” September 6, 2019.
Insurance Coverage
A woman’s insurance status is also likely to impact her health and the care she receives before, during, and after pregnancy, which affects her likelihood of having a healthy pregnancy and delivery and of receiving necessary care after birth. Women receiving no prenatal care are three to four times more likely to have a pregnancy-related death than women who receive prenatal care.[18] Studies have shown that uninsured women and women covered by Medicaid are much less likely to receive adequate prenatal and postnatal care: According to the Medicaid and CHIP Payment Advisory Commission (MACPAC), only 64.2 percent of women covered by Medicaid and 35.7 percent of uninsured women received adequate prenatal care, compared with 84.1 percent of privately insured women between 2012 and 2014.[19] This disparity results from both a difficulty in finding Medicaid providers who will accept new patients and low-income women being less likely to understand the importance of pre- and post-natal care.
Over time, Medicaid has covered a growing share of births in the country, covering more than 47 percent of all births in 2017.[20] This rise is partially due to changes to Medicaid law in the 1980s that require state Medicaid programs to cover pregnant women with income up to 133 percent of the federal poverty level during their pregnancy and up to 60 days following the end of the pregnancy.[21] Further, while only 3 percent of women were uninsured during pregnancy and delivery, 18.8 percent of women were uninsured in the month prior to pregnancy—meaning they were likely not addressing all of their medical needs before becoming pregnant—and 14 percent of women became uninsured again following delivery, which is when most maternal deaths occur.[22]
Insurance coverage and reimbursement rates may also influence whether a woman has a c-section, and perhaps unsurprisingly those with Medicaid or without any insurance at all are less likely to have a c-section. Between 2012 and 2014, 28.4 percent of pregnant women covered by Medicaid delivered via c-section; 14.4 percent of uninsured pregnant women had c-sections. Based on an overall c-section rate of 33 percent, privately insured women must have a c-section rate of more than 37 percent. One study found that women with non-HMO commercial insurance coverage were statistically more likely to have an elective c-section than women covered by Medicaid, an HMO plan, or uninsured, although the rate was still just 0.9 percent in 2007 among women without any indication for pre-labor cesarean delivery.[23] Reimbursement rates could drive this trend: The average charge for a c-section without complications and newborn care is $51,125 in 2013 before insurance, compared to $32,093 for an uncomplicated vaginal delivery and newborn care also before insurance.[24]
Age of Pregnant Women
A woman’s age is another strong indicator of a woman’s risk for complication and death resulting from pregnancy, and age is also related to the other factors discussed above. Most countries show a J-shaped pattern of maternal-mortality risk, with adolescents having a greater risk of maternal mortality than women in their twenties but women over 35 having the greatest risk.[25]
There are a multitude of factors contributing to higher risks for younger women, including an individual’s income, insurance status, and awareness regarding healthy behaviors during pregnancy, which is likely the cause for the increased MMR among adolescents. Women who were uninsured or covered by Medicaid when they gave birth were much more likely, relative to privately insured women, to be low-income, have less education, and be younger than 19.
The higher MMR for older women is likely more related to biological factors. It is well-documented that women over 30 have a greater risk of complications during pregnancy, and women over 35 have the highest MMR.[26] The data have also consistently shown that older women are also more likely to have c-sections, and in 2017, 40.2 percent of deliveries among women aged 35-39 occurred via c-section, while the share for women aged 20-24 was 25.9 percent.[27]
The rising age of mothers is likely contributing to rising MMR, as the risk of complications and death associated with c-sections, as well as the prevalence of chronic conditions, increases with a mother’s age. Between 2007 and 2017, the average age of mothers at first birth rose by 1.3 years to 24.5 in rural areas and by 1.8 years to 27.7 in large metropolitan areas.[28] Further, the birth rate for all age groups younger than 35 declined between 2017 and 2018, while the birth rate for all age groups 35 and older increased.[29] In general, however, increasing age of pregnant women is not a factor that is unique to the United States compared to OECD countries.
Racial/Ethnic Disparities
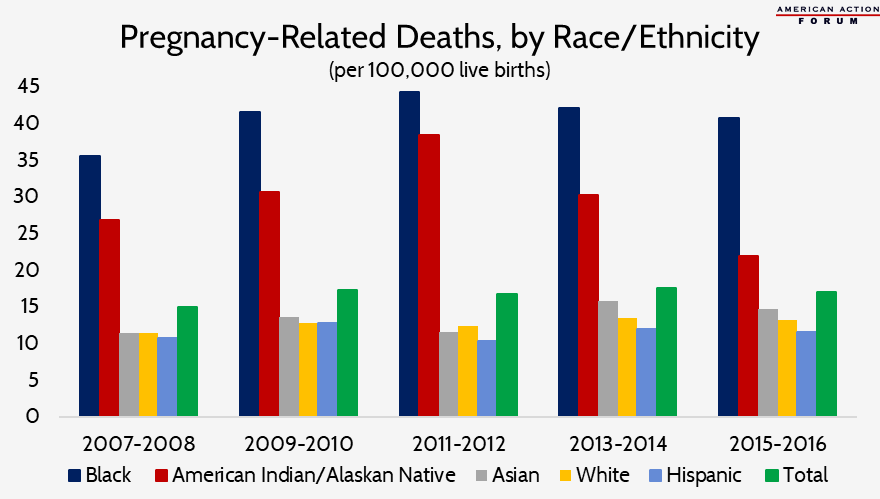
Racial disparities are driving greater maternal mortality and morbidity prevalence among certain populations relative to others. African American and Native American/Alaskan Native women are three to four times more likely to die from pregnancy-related issues than both Hispanic and white non-Hispanic women.[30] The graph below emphasizes the notable differences in mortality rates across different racial/ethnic groups, which persist at all ages—and actually worsen—as education level increases, even in states with the lowest MMR.[31]
Source: Centers for Disease Control and Prevention. “Racial/Ethnic Disparities in Pregnancy-Related Deaths—United States, 2007-2016.” September 6, 2019.
Limited access to quality hospitals and poor or nonexistent prenatal and postnatal care is resulting in poor outcomes. A 2010 Healthy People report found that approximately 25 percent of all pregnant women in the United States do not receive the recommended number of prenatal visits, though, the rates are much higher for minority women: 32 percent of African American women and 41 percent of American Indian/Alaskan Native women do not receive proper prenatal care.[32] This lack of access to early care may be particularly problematic for black women, as African Americans have a higher prevalence of high blood pressure, heart disease, and diabetes, all of which, as mentioned earlier, can cause complications during pregnancy, and may even be fatal if not addressed early or left untreated.[33]
Further, black women giving birth at hospitals predominantly serving minorities are at a higher risk. A study published in 2017 found that 74 percent of black babies were born at the 25 percent of hospitals serving the highest proportion of black individuals, and women delivering at these hospitals were significantly more likely to suffer severe complications than women delivering at lower black-serving hospitals, even after adjusting for patient characteristics and comorbidities.[34] The study author concludes that delivery hospital accounts for nearly half of the difference between black and white maternal mortality rates.
Various other factors likely are contributing to rising MMR among black women. Social determinants of health are likely contributing to the mortality rates experienced by these populations, though the data shows the MMR is higher for black women than white women at every education level. In fact, black women with a college degree were still 2.4 times more likely to suffer severe maternal morbidity and 1.6 times more likely to die from a pregnancy-related complication than a white woman with less than a high school education.[35] For women with a college degree or higher, the disparity ratio is 5.2.[36] The rural-urban divide may also be contributing to the racial disparities. Women in rural areas are at increased risk of lacking access to proper care. A study in 2017 found that more than half of all rural counties in the United States, with 2.4 million women of reproductive age, have no hospital obstetric services and also face primary-care physician shortages.[37] The study found these counties were more likely to have a higher percentage of non-Hispanic black women, to have lower median household incomes, and to be in states with more restrictive Medicaid eligibility. Closing the gaps on these factors is going to be a necessary step in ameliorating the overall maternal mortality rate.
Policy Solutions
A good place to start for improving maternal mortality would be to increase monitoring of and adherence to safety recommendations and best practices developed by the Joint Commission or the Alliance for Innovation on Maternal Health Program, which the American College of Obstetrics and Gynecologists and other provider groups created. A recent investigation found a severe lack of attention to even basic safety protocols for mothers; for instance, fewer than 15 percent of pregnant women at risk of a stroke due to high blood pressure were treated according to recommendations.[38] Interventions such as coordinated care, home visits particularly for at-risk women, health education, prenatal care consultations, and specialized-care referrals can also benefit expecting and postpartum mothers.[39] Increasing insurance coverage, reducing cost restrictions, and pursuing proven provider collaboration models will likely expand access to prenatal and postnatal care. For the uninsured, the average cost of prenatal care is roughly $2,000 in aggregate.[40] Delivery and postnatal care can cost upwards of $15,000, depending on insurance coverage, although this figure does not account for the additional costs associated with bringing a baby home, highlighting the cost burden that is particularly felt by low-income and uninsured.
The Preventing Maternal Deaths Act, signed into law in December 2018, provides federal grants to states for investigating the deaths of women who die within a year of pregnancy.[41] This legislation establishes and supports new and existing state maternal mortality review committees (MMRCs), which are entities that collect and report standardized data on maternal deaths to inform quality improvement interventions, most notably, among other responsibilities.[42] MMRCs also evaluate factors such as social determinants, including racism, economic status, and nutrition to paint a bigger picture of the issues influencing maternal deaths. Drawing from the data, MMRCs develop recommendations and strategies to reduce problematic behaviors and better support women. Various public-private partnerships between state agencies and private stakeholders (payers, providers, hospitals, etc.) focus on realizing these strategic actions. A recent study in Health Affairs found that 38 states currently have active MMRCs recognized by the CDC, with more states in the process of authorizing and establishing additional MMRCs. The funding and supplementary resources provided to the states by the Preventing Maternal Deaths Act allows states to further develop comprehensive data reporting and reduce variability across MMRCs.
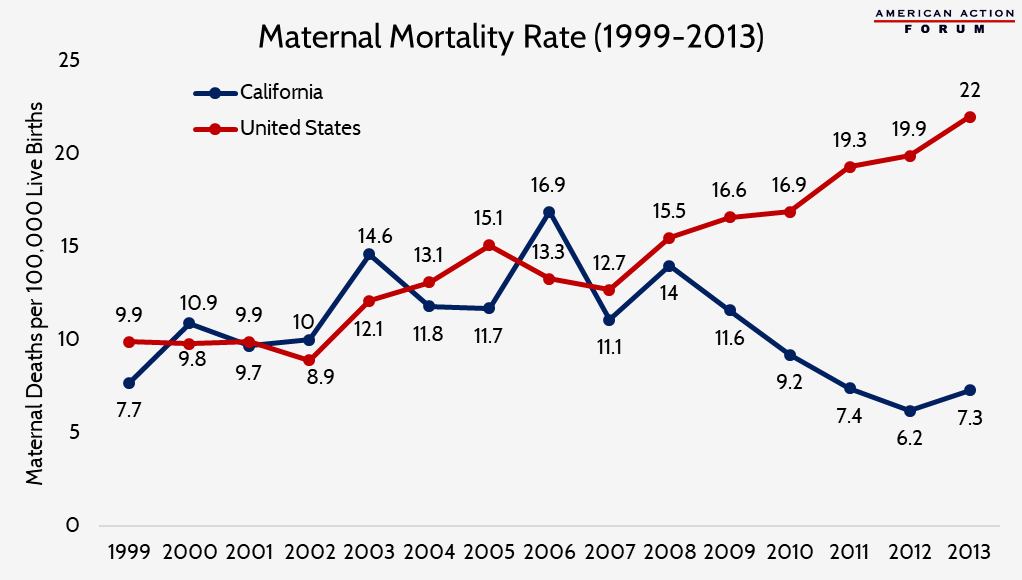
Case Study: California
California has been a pioneer in reducing maternal mortality for over a decade following the implementation of the California Maternal Quality Care Collaborative (CMQCC) in 2006. By 2013, the state’s maternal mortality rate was reduced by half to an average of 7 deaths per 100,000 live births.[43] This trend diverges greatly from the national average, which, according to the CMQCC, rose from 13.3 to 22 deaths per 100,000 during the same time period.[44] Notably, most of the reduction was driven by reduced mortality rates among black women, and while a disparity between blacks and other races still exists in the state, the difference has significantly declined since the program’s creation.[45]
This collaboration between hospitals, clinicians, state agencies, insurers, patient and public groups, and other stakeholders requires four key components: linking public health surveillance and proactive action; mobilizing collaborative public and private partnerships; creating a data system with low administrative burden to support improvements; and establishing multi-stakeholder interventions that connect providers with relevant health services.[46]
Source: State of California, Department of Public Health, California Birth and Death Statistical Master Files, 1999-2013. https://www.cmqcc.org/research/ca-pamr-maternal-mortality-review
The CMQCC and the California Department of Public Health hold annual maternal mortality review committee meetings to assess maternal mortality in the state, including causes of death and demographic characteristics, to determine potential interventions to eliminate mortality among various populations.[47] Recommendations are then used to develop free evidence-based toolkits for stakeholders to implement effective quality improvement strategies.[48] These toolkits inform providers of what to do when complications arise and how to be more equitable and efficient in care delivery.
The most notable difference between California and other states is the success of its Maternal Data Center (MDC), which was created to generate rapid-cycle performance metrics on the maternity care services that patients receive at participating hospitals in order to provide insight and aid in quality improvement efforts. Launched in 2012, over 200 California hospitals representing more than 95 percent of births are monitored by the MDC, with expansions in Oregon (2014) and Washington state (2015).[49] This tool has allowed these hospitals to use real-time data to generate perinatal quality metrics and evaluate performance to meet and exceed established benchmarks while reducing data quality issues and discrepancies in performance reporting.[50]
The combination of mortality reviews, stakeholder engagement, and data has provided a blueprint for improvements targeting performance and quality metrics. The implementation of these large-scale interventions is likely the driving force behind California’s improvements in maternal mortality rates and could potentially have similar effects if administered at the national level across various states to aid in maternal mortality rate reductions. Of course, there are potential limitations and challenges to applying this model, including its reliance upon multi-stakeholder engagement. Under-resourced states may find it difficult to finance data collection and reporting if the infrastructure does not already exist. Rural areas, and especially states that are not receiving enhanced federal funding from expanding their Medicaid programs, may also be unable to support the types of performance initiatives implemented under CMQCC due to more limited access to maternal care services among their uninsured populations (whose rates are higher than in states that have expanded Medicaid) and provider shortages. The Washington Post reports that the cost of California’s efforts to the state Department of Public Health is approximately $950,000 annually, with additional resources from grants and foundations provided.
Case Study: North Carolina
North Carolina also implemented some statewide initiatives to address maternal mortality over the past decade and has seen some improvements. In 2009, North Carolina implemented the Perinatal Quality Collaborative, working with 65 hospitals across the state to improve quality by changing care practices, such as reducing the number of early elective deliveries. In 2011, the state created a new Medicaid Pregnancy Medical Home, which sought to improve care coordination, particularly among low-income individuals, similar to what California did. Medicaid providers are financially incentivized to screen for conditions that might put a woman at higher risk for complications during pregnancy; if risk is found, she is referred to a case manager who can help monitor her care and make sure she understands not just what she needs to be doing, but also why. The case manager will also visit their patients at home and assist in overcoming nonmedical challenges that may affect the health of mom and baby, such as food insecurity or housing issues.
These efforts seem to be contributing to improved outcomes and reduced MMR for black women in the state, so much so that the disparity between black and white women was virtually eliminated in 2013. Though, the elimination of that gap was not achieved as a result of the MMR for black women falling compared to the MMR for white women when these interventions began.[51] Rather, unlike in California, the MMR for white women in North Carolina has been increasing, similar to the overall national rate. It is unclear why black women are seeing such a benefit, but not white women. White women comprise a greater share of North Carolina’s Medicaid population than black women: 43 percent, compared with 37 percent, according to the most recent figures.[52]
Conclusion
Addressing maternal mortality in the United States will require more than infrastructural improvements to better track the causes of deaths. Policymakers and providers need to recognize the influence of social determinants and health inequities to create more far-reaching policies to target the most vulnerable populations. The last year has seen an uptick in legislation intending to tackle these crucial issues, but the work is certainly not done. Fortunately, California has provided a model for other states to follow, though each state will likely need to adapt its strategy to their population’s specific needs.
[1] https://www.who.int/healthinfo/statistics/indmaternalmortality/en/
[2] https://www.cdc.gov/reproductivehealth/maternalinfanthealth/pregnancy-mortality-surveillance-system.htm
[3] https://www.cmqcc.org/research/ca-pamr-maternal-mortality-review, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5001799/
[4] https://www.cdc.gov/mmwr/volumes/68/wr/mm6818e1.htm?s_cid=mm6818e1_w
[5] https://www.cdc.gov/reproductivehealth/maternalinfanthealth/severematernalmorbidity.html
[6] https://www.smithsonianmag.com/smart-news/cdc-says-more-half-us-pregnancy-related-deaths-are-preventable-180972140/
[7] https://www.cdc.gov/mmwr/volumes/68/wr/mm6818e1.htm?s_cid=mm6818e1_w, https://apps.who.int/iris/bitstream/handle/10665/194254/9789241565141_eng.pdf;jsessionid=A5BCC05853070F3E0AAADCC3FB3CB6EB?sequence=1, https://stats.oecd.org/index.aspx?queryid=30116
[8] https://www.usnews.com/news/healthiest-communities/articles/2019-05-07/most-pregnancy-related-deaths-preventable-cdc-says
[9] https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(18)31928-7/fulltext
[10] https://www.mayoclinic.org/tests-procedures/c-section/about/pac-20393655
[11] https://www.nytimes.com/2019/03/05/well/family/reducing-maternal-mortality.html#
[12] https://www.healthaffairs.org/doi/full/10.1377/hlthaff.2012.1030
[13] https://www.mayoclinic.org/tests-procedures/c-section/about/pac-20393655
[14] https://www.reuters.com/article/us-health-cesarean/c-section-complication-risk-rises-with-mothers-age-idUSKCN1RN2SN
[15] https://medicalxpress.com/news/2017-11-chronic-conditions-moms-babies.html
[16] https://medicalxpress.com/news/2017-11-chronic-conditions-moms-babies.html
[17] https://www.usnews.com/news/healthiest-communities/articles/2019-05-07/most-pregnancy-related-deaths-preventable-cdc-says
[18] https://www.mhtf.org/topics/maternal-health-in-the-united-states/
[19] https://www.macpac.gov/wp-content/uploads/2018/11/Pregnant-Women-and-Medicaid.pdf
[20] http://files.kff.org/attachment/Report-Implementing-Coverage-and-Payment-Initiatives
[21] http://files.kff.org/attachment/Report-Medicaid-Coverage-of-Pregnancy-and-Perinatal-Benefits
[22] https://www.macpac.gov/wp-content/uploads/2018/11/Pregnant-Women-and-Medicaid.pdf, https://docs.house.gov/meetings/WM/WM00/20190516/109496/HHRG-116-WM00-Wstate-HarrisP-20190516.pdf
[23] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3222406/
[24] https://www.theguardian.com/us-news/2018/jan/16/why-does-it-cost-32093-just-to-give-birth-in-america
[25] https://www.thelancet.com/journals/langlo/article/PIIS2214-109X(14)70007-5/fulltext
[26] https://www.urmc.rochester.edu/encyclopedia/content.aspx?contenttypeid=90&contentid=P02481, https://www.thelancet.com/journals/langlo/article/PIIS2214-109X(14)70007-5/fulltext
[27] https://www.statista.com/statistics/206438/us-cesarean-delivery-rates-by-age-of-mother/
[28] https://www.cdc.gov/nchs/products/databriefs/db323.htm
[29] https://www.cdc.gov/nchs/data/vsrr/vsrr-007-508.pdf
[30] https://www.smithsonianmag.com/smart-news/cdc-says-more-half-us-pregnancy-related-deaths-are-preventable-180972140/
[31] https://www.cdc.gov/mmwr/volumes/68/wr/mm6835a3.htm
[32] https://www.cdc.gov/nchs/data/hpdata2010/hp2010_final_review.pdf
[34] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4698019/
[35] https://www.ucsfcme.com/2018/MOB18003/SLIDES/13_HOWELL_Racial_Ethnic_Disparities_Maternal_Mortality.pdf, https://www.cdc.gov/mmwr/volumes/68/wr/mm6835a3.htm
[36] https://www.cdc.gov/mmwr/volumes/68/wr/mm6835a3.htm
[37] https://www.healthaffairs.org/doi/10.1377/hlthaff.2017.0338
[38] https://www.advisory.com/daily-briefing/2018/07/31/childbirth
[39] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6048753/
[40] https://www.webmd.com/baby/features/cost-of-having-a-baby#1
[41] https://www.nytimes.com/2019/03/05/well/family/reducing-maternal-mortality.html#
[42] https://www.healthaffairs.org/do/10.1377/hblog20190130.914004/full/
[43] https://www-healthaffairs-org.proxy-um.researchport.umd.edu/doi/10.1377/hlthaff.2018.0463
[44] https://www.washingtonpost.com/national/health-science/a-shocking-number-of-us-women-still-die-from-childbirth-california-is-doing-something-about-that/2018/11/02/11042036-d7af-11e8-a10f-b51546b10756_story.html?utm_term=.30aea82465de
[45] https://www.publichealthpost.org/databyte/disparities-maternal-mortality-california/
[46] https://www-healthaffairs-org.proxy-um.researchport.umd.edu/doi/10.1377/hlthaff.2018.0463
[47] https://www-healthaffairs-org.proxy-um.researchport.umd.edu/doi/10.1377/hlthaff.2018.0463
[48] https://www-healthaffairs-org.proxy-um.researchport.umd.edu/doi/10.1377/hlthaff.2018.0463
[49] https://www.cmqcc.org/maternal-data-center
[50] https://www.cmqcc.org/maternal-data-center
[51] https://schs.dph.ncdhhs.gov/data/maternal/Table4_MMReport2013.pdf
[52] https://www.kff.org/medicaid/state-indicator/medicaid-enrollment-by-raceethnicity/?currentTimeframe=0&selectedRows=%7B%22states%22:%7B%22north-carolina%22:%7B%7D%7D%7D&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D