Research
June 5, 2025
Vaccine Protection and Productivity: The Economic Value of Vaccines
Executive Summary
- The creation, development, and deployment of vaccines – a U.S. federal priority since the 1960s – has been one of the greatest health care achievements in the world.
- Routine childhood immunizations in the United States from 1994–2023 are estimated to have prevented around 508 million cases of illness, 32 million hospitalizations, and more than 1 million deaths; adult vaccinations have a significant role in safeguarding public health and considerable economic benefits through reducing absenteeism, addressing presenteeism, and enhancing overall labor productivity.
- For child vaccinations, this prevention results in approximately $540 billion in direct medical cost savings, with almost $2.7 trillion in total societal savings due to illness prevention, which means that every $1 spent on childhood immunizations results in a savings of approximately $11; in adults, one study calculated that an adult vaccination program can return up to 19 times its initial investment.
Introduction
Immunizations are one of the most significant and effective innovations in protecting public health in America. They have saved millions of lives and drastically reduced, eliminated, or eradicated deadly and debilitating infectious diseases like polio and measles. In addition to preventing a staggering human cost of disease, vaccines have resulted in trillions of dollars in direct and indirect societal savings. They are one of the best investments America can make in economic productivity.
Both childhood and adult vaccinations create high resultant returns on investment. This return on investment is not theoretical. Vaccines have been studied for their contribution to current and future labor productivity, with many studies concluding that any vaccination, at any age, creates economic value.
Childhood Vaccinations
Ensuring that children have access to safe, effective vaccines has been a priority of federal health policy since the 1960s, when President John F. Kennedy signed the Vaccine Assistance Act to create a federal support system for vaccinations in states and communities. That support has since manifested as the Vaccines for Children (VFC) program, established in statute by Congress in 1993 in response to the 1989–1991 measles epidemic and operationalized in 1994 by the Centers for Disease Control and Prevention (CDC). The VFC program provides free vaccines to children who might otherwise lack access due to financial constraints. Over the past three decades, the program has not only improved public health outcomes but also demonstrated a significant return on investment for the United States.
Reductions in morbidity should be enough to demonstrate that vaccinations make the United States healthier, but it goes beyond simply making Americans less likely to get sick. Vaccines significantly reduce direct health care expenditures by preventing diseases before they occur. This preventive approach is much more cost-effective than treatment-based strategies. For instance, routine childhood immunizations in the United States from 1994–2023 are estimated to have prevented around 508 million cases of illness, 32 million hospitalizations, and 1.13 million deaths. Translated to dollars, this prevention results in approximately $540 billion in direct medical cost savings, with almost $2.7 trillion in total societal savings due to illness prevention. This calculation means that every $1 spent on general childhood immunization resulted in a savings of approximately $11.
The economic impact of vaccinations extends into the educational domain as well. Healthy children experience fewer disruptions in their schooling, which leads to improved academic performance, higher educational attainment, and better cognitive development. Long-term studies have linked early-life vaccinations to increased earnings in adulthood, suggesting that healthier children become more productive adults. This intergenerational benefit reinforces economic stability and growth.
Adult Immunizations
The benefits of vaccinations are not limited to children. Adult vaccinations play a significant role in safeguarding public health and have considerable economic implications through reducing absenteeism, addressing presenteeism, and enhancing overall productivity. A study from the Office of Health Economics calculated that an adult vaccination program can return up to 19 times its initial investment.
Seasonal vaccines, including annual influenza vaccinations and booster shots for diseases such as COVID-19, not only protect individual health but also benefit employers and the broader economy by maintaining a healthier, more productive workforce.
One of the most immediate economic benefits of adult vaccinations is the reduction of absenteeism – the absence of employees from work due to illness. Seasonal flu, for example, is known to lead to substantial work loss annually, with the Centers for Disease Control and Prevention (CDC) estimating that influenza contributes to approximately 17 million workdays lost each flu season in the United States alone. By contrast, widespread flu vaccination among adults has been shown to substantially decrease this number, with studies indicating a 40–60 percent reduction in influenza-related absenteeism among vaccinated populations. Such reductions directly translate into economic savings for businesses in terms of lower temporary worker replacement costs and decreased disruption to productivity and workflow.
Moreover, vaccines also reduce the problem of presenteeism, which occurs when employees come to work despite illness, resulting in decreased productivity and potential spread of infection among coworkers. Presenteeism is often harder to measure but can be as or more costly than absenteeism. Research published in the Journal of Occupational and Environmental Medicine highlights that presenteeism due to influenza-like illnesses can reduce individual employee productivity by as much as 30–50 percent. By promoting adult vaccination, employers mitigate these risks, thereby enhancing productivity and reducing indirect costs associated with diminished workplace performance.
The broader impact on labor productivity gains from adult vaccinations is also substantial. Healthy employees perform better, contribute more effectively, and sustain fewer interruptions in their tasks. According to economic analyses, the aggregate productivity benefits of adult vaccinations extend beyond immediate reductions in absenteeism and presenteeism. For instance, comprehensive immunization programs, including booster shots for COVID-19 and influenza vaccines, are estimated to return significant economic value, with some studies suggesting returns ranging between $2–4 for every $1 invested due to improved worker productivity and reduced health care costs.
The COVID-19 pandemic underscored this economic dynamic, with booster shots playing a critical role in maintaining workforce stability. Employers witnessed firsthand the significant disruptions caused by illness-related absenteeism and presenteeism during the pandemic’s peak. Companies that proactively supported vaccination and booster initiatives experienced better continuity, fewer operational disruptions, and more robust economic performance. Vaccinated workers generally require fewer medical interventions and hospitalization, translating to lower overall health care expenditures for employers and insurers alike.
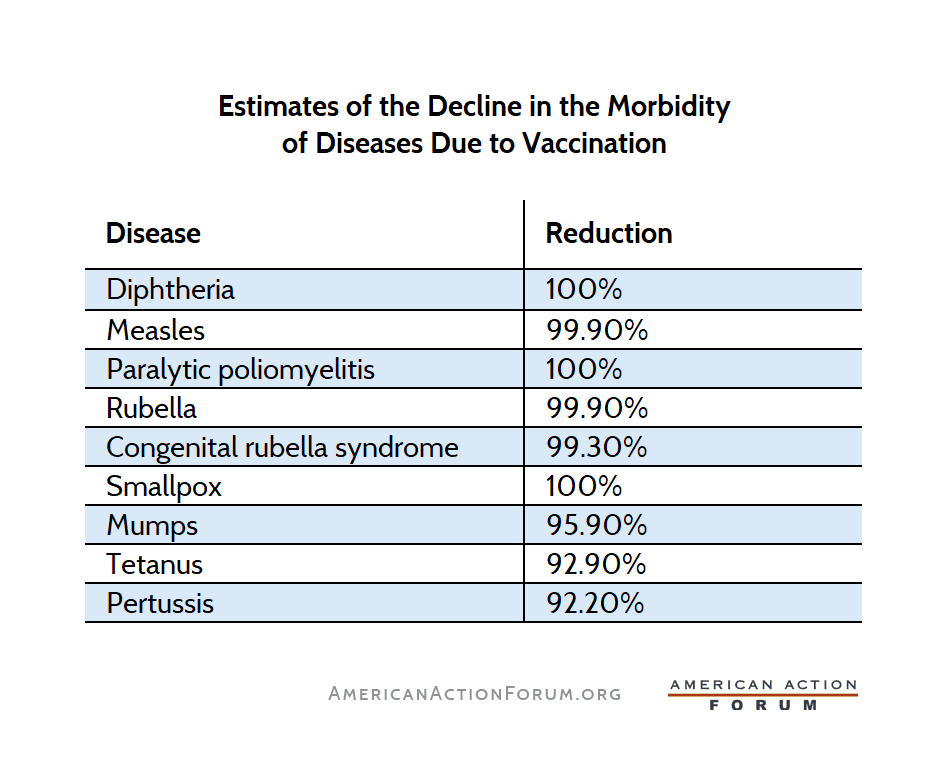
Below is a sample of the impact that routine vaccinations can have on disease morbidity (having or being affected by a disease).
Source: Immunization in the United States: Recommendations, Barriers, and Measures to Improve Compliance
Extensive research has been conducted on the value of vaccines. The three case studies below demonstrate the value of vaccinations, and the costs associated with the lack of vaccination.
Measles
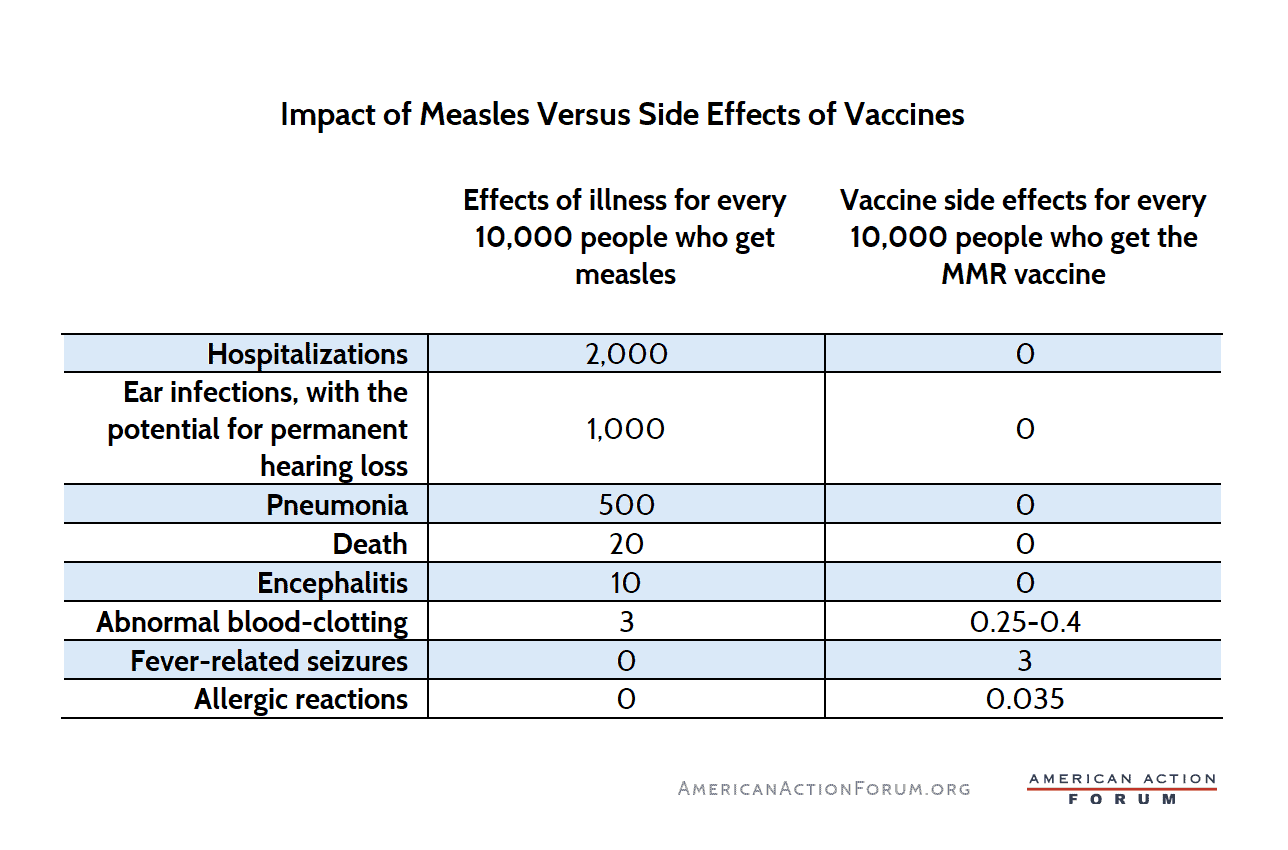
Measles – one of the most contagious diseases in the world – has recently been in the news and has underscored the importance of maintaining high vaccination coverage. The MMR vaccine is one of the most effective vaccines in the world, with two doses of the vaccine, administered according to expert recommendations, proving 97 percent effective against measles. This is important because of the debilitating – and sometimes deadly – effects of the disease.
Source: The New York Times
Routine measles vaccination in the United States costs between $20–70 per dose, including administration. Despite these modest costs, the savings from the avoided disease burden are substantial. A 2014 CDC analysis estimated that every dollar spent on the MMR vaccine saves the U.S. health care system $13.50 in direct and indirect costs, including avoided hospitalizations, lost productivity, and outbreak response expenditures.
The economic consequences of outbreaks are significant. “Each measles case can be $30,000 to $50,000 for public health response work, and that adds up quite quickly,” said Dr. David Sugerman, a senior measles scientist at the CDC. This includes testing, laboratory work, contact tracing, vaccination efforts and health care costs, according to Dr. Catherine Troisi, an infectious disease epidemiologist with UTHealth Houston. Notably, this doesn’t include hospitalizations, which for measles can range anywhere from $5,000 to more than $20,000 per patient, especially if complications arise.
During the 2014 measles outbreak linked to Disneyland, the direct public health response cost nearly $1 million, excluding the cost of health care for infected individuals. The 2019 Clark County, Washington measles outbreak cost $3.4 million ($47,479 per case or $814 per contact), with productivity losses alone contributing over $1 million to this cost. The response to the ongoing measles outbreak in Texas is also proving costly, in large part due to the number of hospitalizations that have occurred. As of April 2025, the Texas Department of Health and Human Services announced the outbreak has cost taxpayers $4.5 million. These have been predominately in direct medical costs, and indirect societal and productivity costs won’t be known until adequate research has been conducted.
As indicated by this trend, containing, treating, and re-eliminating measles outbreaks has become increasingly expensive. This is due to several reasons, but the predominant reason is the decreasing vaccination rate. As more individuals are unvaccinated, the size and severity of outbreaks will continue to grow, which further accelerates the cost of outbreaks.
Varicella (Chickenpox)
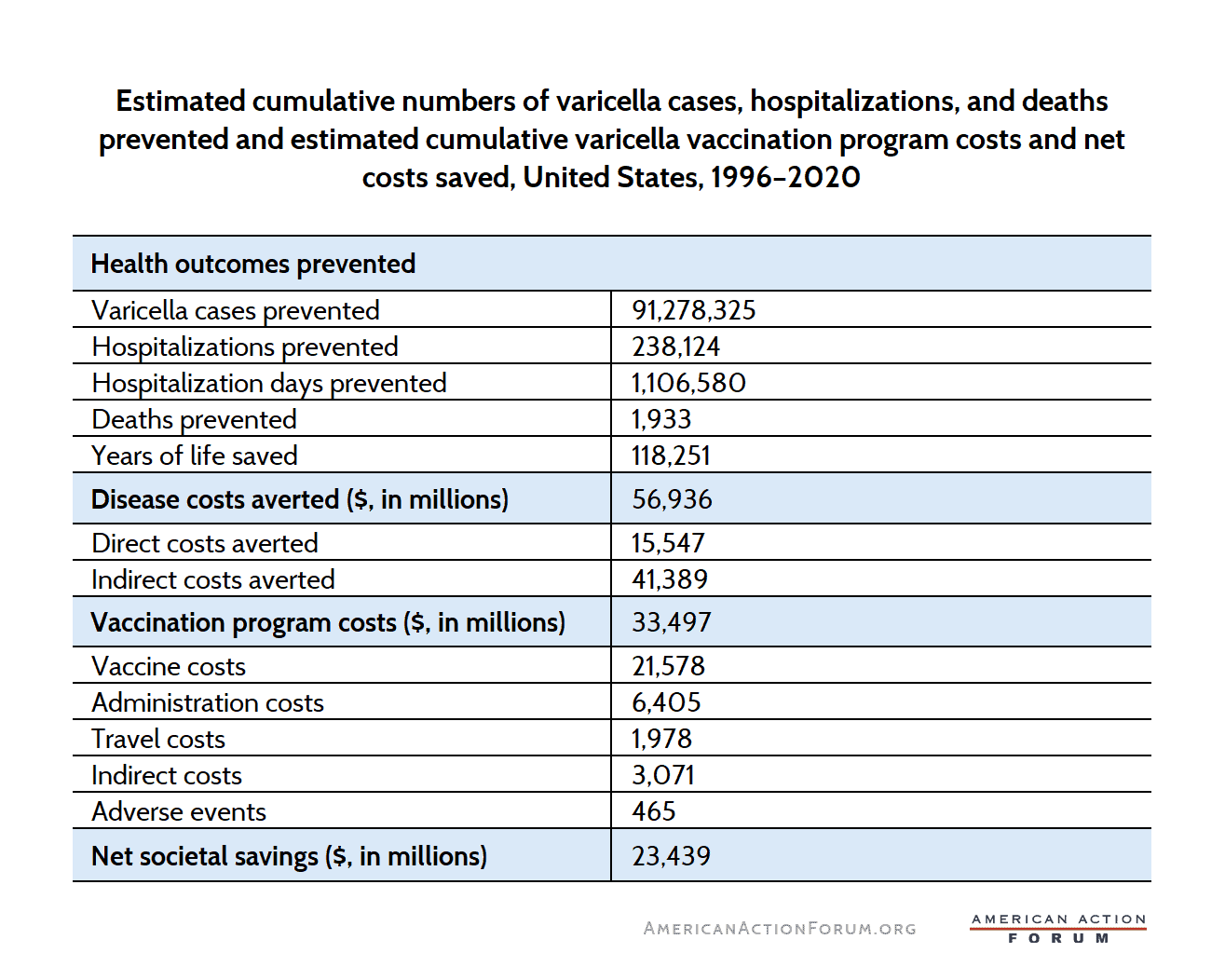
Many adults will remember varicella (chickenpox), either because they got the disease themselves or because their children did. In 1995, a vaccine was approved and began to roll out across the country. The United States implemented a varicella vaccination program from 1996–2020 to control the disease and prevent the approximately 4 million cases of chickenpox that occurred every year. These immunizations also generated significant economic benefits, achieving net societal savings estimated at $23.4 billion. Conducted from a comprehensive societal perspective, the analysis evaluated direct and indirect economic savings by comparing outcomes from the vaccination era to those prior to vaccine implementation (1990–1994). Over the 25-year span, the program successfully prevented approximately 91 million cases of varicella, 238,000 hospitalizations, and nearly 2,000 premature deaths, saving an estimated 118,000 life-years.
The economic benefits primarily stem from reduced indirect costs associated with productivity losses due to illness or caregiving, totaling $41.4 billion. Direct medical cost savings amounted to approximately $15.5 billion, reflecting substantial reductions in health care utilization, including fewer outpatient visits and hospitalizations. The total cost of implementing the vaccination program was approximately $33.5 billion, encompassing vaccine procurement, administration, travel expenses for vaccinations, and management of minor adverse events.
Source: Journal of Infectious Diseases.
For every dollar invested, the program generated $1.70 in societal savings, underscoring its economic efficiency. Additionally, the program contributed to reducing health disparities by improving vaccine access. Overall, the varicella vaccination initiative exemplifies a highly effective public health strategy, yielding substantial long-term economic and health benefits for the United States.
An important realization is that prevention of a varicella infection is not only about preventing a case of chickenpox. The varicella zoster virus that causes the disease is also responsible for developing into shingles. Shingles occurs because of declining immunity, when the varicella-zoster virus reactivates in patients after they have already had chickenpox. Shingles affects nearly one in three people, a risk that increases with age. While receiving the varicella vaccine does not explicitly reduce the likelihood of developing shingles later in life, it does provide a more effective starting point for the prevention of shingles than that of an unimmunized individual.
Shingles, which manifests with painful symptoms, can be debilitating and greatly reduce quality of life, with significant loss of independence in some cases. This is often due to postherpetic neuralgia, which can affect individuals years after visible symptoms (such as the trademark rash) have subsided. Shingles is associated with the loss of more than 60,000 quality of life years and $2.4 billion annually in direct medical costs and productivity losses in the United States. Receiving a shingles vaccine is the most effective method of protecting oneself against developing shingles and lessening the loss of quality life years and economic productivity.
Tetanus
Tetanus, although rare in developed countries, leads to severe health outcomes, including hospitalization, intensive care, and prolonged recovery periods. Tetanus has no cure, and treating cases is costly, often exceeding tens of thousands of dollars per hospitalization, primarily due to the intensive medical care required. Babies and children are recommended to get a series of tetanus shots. Booster shots, recommended every 10 years for adults, continue to drastically reduce the risks of tetanus and prevent costly medical interventions.
Tetanus infection results in substantial absenteeism, as individuals infected typically require lengthy hospitalization and extensive recovery time, often weeks or months. By preventing infections through booster shots, adults maintain their productivity, directly benefiting employers and the broader economy by reducing lost labor hours.
Severe cases of tetanus can lead to long-term disabilities, significantly reducing an individual’s productive capacity and leading to potential lifelong economic losses. Disability places financial strain not only on individuals but also on public health systems, social safety nets, and families providing long-term care. Regular tetanus boosters mitigate these risks, preserving workforce capability and economic productivity.
Initial vaccination as a child and widespread adherence to tetanus boosters contributes to broader public health resilience, stabilizing health care infrastructure and resources. In scenarios involving disasters or emergencies, vaccination status becomes crucial to prevent tetanus infections due to contaminated injuries, thus ensuring economic and societal stability in times of crisis.
Tetanus is rare due to widespread vaccination, but when cases occur, the economic burden is high. Regular booster vaccinations prevent substantial medical costs.
Incremental Cost
As U.S. policymakers aim to continue designing immunization outreach and administration programs, they may ask: How much does it cost to increase vaccine coverage, especially among hard-to-reach populations? According to some research, the average cost to improve immunization by just 1 percent ranged from as low as $0.01–$38.16 per dose, with a mean of $3.13.
The United States – which deeply desires value in health care – can get a lot of value out of increasing immunizations in vaccine-preventable diseases. Campaign-based interventions were generally more cost-effective than routine immunization approaches, averaging $1.37 per dose, per percentage point gain in coverage. One should acknowledge that the closer a community gets to full coverage, the more expensive each additional point gained becomes. But as previously discussed, an approximate calculation shows that every $1 spent on childhood immunizations results in a savings of approximately $11. This return on investment (roughly 700 percent) seems to be well worth the incremental costs, even as the “last mile” coverage gets slightly more expensive.
Lasting Value From Childhood Investment
The benefits of childhood vaccination do not suddenly stop when someone turns 18. Long-lasting immune protection (such as from the MMR and varicella vaccines) continues to provide benefits into adulthood and impacts many aspects of life, including parenting and workplace productivity. Diseases such as measles and meningitis can result in chronic health issues and disabilities, which may significantly reduce lifetime productivity.
Vaccines for rarer diseases generally address conditions that, though uncommon, are severe or fatal. The economic and societal value in preventing these outcomes justifies vaccination investments. Vaccination protects communities, maintaining healthcare resources and reducing the economic disruption associated with outbreaks or isolated cases of rarer but severe diseases. There are several recognizable examples of these types of diseases, both of which are generally vaccinated against as children or adolescents.
Meningococcal infections, while rare, have catastrophic health outcomes, including death or permanent disability. Vaccination provides substantial economic benefit by preventing these severe outcomes. A U.S.-based economic evaluation estimated that routine meningococcal vaccination for adolescents generates cost-effectiveness ratios between $105,000-$269,000 per Quality-Adjusted Life Year (QALY) gained. While these estimations are primarily based on a single-dose regimen, the productivity gains are amplified if a two-dose strategy is followed. If public health vaccination campaigns work toward reaching adolescent and adult populations for meningococcal vaccines, QALYs gained reach to a cumulative $9.2–$12.7 million.
Though human papillomavirus (HPV)-related cancers may be considered relatively uncommon, more than 85 percent of people will get an HPV infection in their lifetime. The CDC notes HPV vaccination could prevent over 33,000 cases of HPV-related cancers annually, translating into billions of dollars in healthcare cost savings over time.
Even small numbers of rarer disease cases can generate significant cumulative costs due to hospitalization, intensive care, rehabilitation, and lifelong disability support.
Vaccinations also enhance presenteeism, the effectiveness of workers who remain on the job despite being ill. Even mild illnesses can markedly reduce workers’ productivity, negatively impacting business operations. A study in Japan showed annualized costs of presenteeism per capita at over $400 USD, with estimated national costs topping $214 billion. According to one report that focused on the United States, absent workers cost companies around $150 billion each year, while those who came to work but weren’t fully functioning due to illness cost $1.5 trillion per year in lost productivity. Each of these numbers alone is noteworthy, but when combined show the enormous cost of illness to the U.S. economy. While not solely attributed to infectious diseases, immunizations protect workers against severe, potentially disabling illnesses, preserving long-term labor productivity.
Conclusion
Vaccinations prevent long-term productivity losses associated with severe illnesses or permanent disabilities. Diseases such as polio, measles, and meningitis can have lasting impacts, impairing individuals’ ability to participate fully in the workforce. By immunizing populations, societies preserve human capital, maintaining a workforce capable of contributing actively to economic development. The aggregated impact of vaccination is astounding, with millions of lives and billions of dollars saved.