Weekly Checkup
July 23, 2021
Budget Games and the Rebate Rule
Infrastructure is the topic du jour in official Washington, but as is often the case, health policy is finding its way into the discussions. The pharmaceutical industry has been a target of lawmakers looking for ways to offset the costs of both the bipartisan infrastructure package and the partisan reconciliation proposal expected to follow. But in a surprising twist, the latest drug policy reform lawmakers are eyeing as a “payfor” would be welcomed by drug manufacturers. This story is an example of the sort of budget gimmickry that so often attends claims that new spending has been paid for.
Back in February 2019, the Trump Administration issued a proposed rulemaking targeting the rebates that drug manufacturers pay to pharmacy benefit managers (PBMs) to secure preferred placement on insurers’ drug formularies. Manufacturers have long argued that their contracts with PBMs force them to keep list prices high in order to provide large discounts, or rebates, to the PBMs. The details of the policy are described in this American Action Forum (AAF) analysis from 2019, but to briefly summarize, the rule would require that PBMs pass those rebates through directly to the Medicare beneficiary to whom the drug has been dispensed to offset their cost-sharing requirements. Currently the PBM/insurer keeps the rebate and in theory uses it to keep premiums for Medicare drug plans low for all enrollees. The policy would provide relief to seniors with especially high-cost medications but would also likely result in marginal increases in premiums across the board. In effect, a few beneficiaries would receive substantial relief while most would see very small increases in their premiums. Of note, because those premiums are subsidized by the federal government, the Trump Administration projected the rule would cost the federal government $191 billion.
Ultimately the Trump Administration backed down and withdrew the rule, or at least it appeared to. The second part of this saga was a late 2020 effort by the administration to revive the proposed rule in order to make good on former President Trump’s assorted promises to lower drug costs. The administration finalized the rule in November 2020 with minimal revisions, arguing that it hadn’t formally withdrawn the rule, but only said it was withdrawing the rule, so it could bypass the normal rulemaking process in order to implement the policy before the Biden Administration took office. At the time, AAF’s Dan Bosch wrote in detail about these maneuvers, but suffice it to say that the contrived regulatory process placed the final rule on shaky legal ground and resulted in immediate legal action by the PBMs to invalidate it.
Amid the ongoing legal challenges, the Biden Administration moved quickly to delay the rule’s effective date by a year to January 2023, buying itself time to sort out the mess. But in another wrinkle, this rule has found its way into the negotiations over the infrastructure package. Congressional budgetary scorekeeping is a complicated matter, particularly the way the Congressional Budget Office (CBO) treats proposed and final regulatory actions by the executive branch. When an administration proposes rulemaking, CBO includes a portion, in most cases half, of the estimated cost in the federal budget baseline, and when the rule is finalized the entirety of the spending or revenue resulting from the proposal is added to the baseline. Effectively what that means is that while the rebate rule is currently tied up in court where it very well may be struck down, the projected increase in federal spending (which former Secretary of Health and Human Services Alex Azar claimed in writing won’t actually occur) is in the budget baseline. Ergo, if Congress were to repeal the rebate rule as part of an infrastructure bill, it would score as saving money (current estimates are in the neighborhood of $181 billion).
In other words, lawmakers are proposing taking potential future spending that may very well never happen, and spending the same amount of money on whatever is currently passing for infrastructure, all while claiming they haven’t increased federal spending. The merits of the actual rebate policy are beside the point, because the important thing, as always, is gaming the scoring process so you can spend as much money as possible.
Chart Review: Telehealth Disparities
Jake Griffin, Health Care Policy Intern
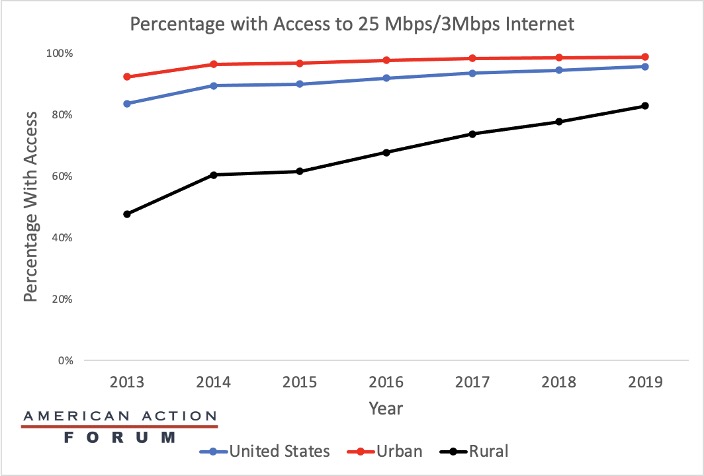
The pandemic has revolutionized the role of telehealth in health care organizations, as it increases social distancing while minimizing the surge of patient demand on facilities. Although policy changes throughout the COVID-19 pandemic have promoted telehealth by reducing barriers to it, geographic disparities continue to exist. Most telehealth services require internet services capable of downloading data at a speed of 25 megabits per second (Mbps) and uploading at a speed of 3 Mbps. As the graph below shows, the percentage of Americans in urban and rural areas with adequate internet service differs. While this gap has decreased between 2013-2019 due to significant improvements in rural areas, nearly a quarter of rural Americans still lack access to internet speeds necessary for efficient telehealth. With telemedicine likely here to stay, efforts to increase internet speeds in rural areas will be important, especially as rural hospitals continue to close in record numbers.
Source: Federal Communications Commission’s 2020 Broadband Deployment Report
Tracking COVID-19 Cases and Vaccinations
Jake Griffin, Health Care Policy Intern
To track the progress in vaccinations, the Weekly Checkup will compile the most relevant statistics for the week, with the seven-day period ending on the Wednesday of each week.
| Week Ending: | New COVID-19 Cases: 7-day average |
Newly Fully Vaccinated: 7-Day Average |
Daily Deaths: 7-Day Average |
| 21-Jul-21 | 40,246 | 166,888 | 223 |
| 14-Jul-21 | 27,443 | 237,405 | 204 |
| 7-Jul-21 | 16,039 | 238,360 | 175 |
| 30-Jun-21 | 13,407 | 317,504 | 225 |
| 23-Jun-21 | 11,788 | 403,788 | 256 |
| 16-Jun-21 | 12,388 | 622,823 | 299 |
| 9-Jun-21 | 15,573 | 726,304 | 357 |
| 2-Jun-21 | 15,000 | 521,321 | 390 |
| 26-May-21 | 22,365 | 818,596 | 459 |
| 19-May-21 | 28,048 | 1,060,555 | 526 |
| 12-May-21 | 34,919 | 1,273,049 | 566 |
| 5-May-21 | 45,511 | 1,468,328 | 597 |
| 28-Apr-21 | 52,328 | 1,503,019 | 626 |
| 21-Apr-21 | 61,253 | 1,523,534 | 638 |
| 14-Apr-21 | 68,663 | 1,776,502 | 645 |
| 7-Apr-21 | 64,244 | 1,602,555 | 625 |
| 31-Mar-21 | 64,039 | 1,387,045 | 733 |
| 24-Mar-21 | 56,946 | 976,605 | 733 |
| 17-Mar-21 | 53,417 | 1,033,582 | 876 |
| 10-Mar-21 | 54,263 | 964,588 | 1,148 |
| 3-Mar-21 | 61,249 | 923,194 | 1,407 |
| 24-Feb-21 | 64,632 | 851,711 | 1,782 |
| 17-Feb-21 | 74,198 | 750,551 | 1,945 |
| 10-Feb-21 | 100,573 | 708,771 | 2,381 |
| 3-Feb-21 | 129,784 | 488,252 | 2,730 |
| 27-Jan-21 | 160,164 | 338,569 | 3,176 |
Sources: Centers for Disease Control and Prevention Trends in COVID-19 Cases and Deaths in the US, and Trends in COVID-19 Vaccinations in the US.
Note: The U.S. population is 332,542,078.
Worth a Look
Reuters: Africa demands local production of COVID vaccines
Wall Street Journal: In Pursuit of a Career in Healthcare, She Became an Engineer