Weekly Checkup
November 20, 2020
The Problems with Trump’s Expected Drug-Policy Rules
Later today the Trump Administration is expected to announce several regulatory actions on drug prices, in a move somewhat akin to trying to write a 40-page term paper the night before it’s due. Among the anticipated items are the rebate rule—aimed at the rebates that drug manufactures pay to Medicare Part D prescription drug plans—and the president’s much-touted, little-explained “most favored nation” (MFN) proposal. It is worth looking at each of these.
The president has long been focused on drug prices. As a candidate in 2016, Trump argued for Medicare to negotiate prices for prescription drugs, a longstanding liberal policy priority that ignores how Medicare’s prescription drug program works. Then, President-elect Trump complained that pharmaceutical companies “are getting away with murder” in relation to the disparity in prices paid in the United States versus other nations. And as recently as July and September, the president signed several executive orders (EOs) on drug prices laying the groundwork for today’s expected announcements.
The president’s underlying concern that Americans pay more for therapies is legitimate. Most other nations actively limit the prices of drugs, but there are real tradeoffs. Patients in other countries face limited access to the newest therapies, and when they do gain access it is months or even years after American patients. Foreign countries are able to limit drug prices for two reasons: First, they are often less committed to the free-market principles critical to maintaining innovation, and second, they are willing to turn down treatments that could address unmet health needs among their populations. American politicians and patients have been unwilling to forego lifesaving medical treatments to save money.
On the merits of these two rules, it’s a mixed bag. The rebate rule would force Medicare Part D plans to pass through any rebates received from drug manufacturers directly to beneficiaries. Currently plan sponsors keep the rebates, arguing that they use the rebates to lower premiums for all beneficiaries enrolled in the plan. Passing the rebates through to patients, however, would dramatically help patients with expensive drug bills, while only modestly increasing premiums for all beneficiaries.
Overall, the rebate rule makes sense, but there are a few issues. First, it may increase federal spending, because Medicare Part D premiums are federally subsidized and could increase, but the president’s EO in July instructed the Department of Health and Human Services (HHS) to modify the proposal so as not to increase federal spending. It’s not clear how HHS can accomplish that while keeping the substance of the underlying policy. An additional wrinkle—explained by the American Action Forum’s Dan Bosch here—is that the administration appears to have withdrawn the original proposed rebate rule. So, the administration would first need to issue a proposed rule. Trump will leave office in January, however, and there isn’t time to follow the legal process for rulemaking, so it appears the administration will just skip most of the steps and call it good.
The other major action will be the MFN rule. Tara Hayes and I detailed what little is known about this rule earlier in the week, as well as its potential impact on innovation. According to the president’s executive order, the rule would require Medicare to pay no more for drugs than the lowest price paid by other members of the Organisation for Economic Co-operation and Development. This is a fancy way of saying that the U.S. government will piggyback on the price-setting schemes of foreign countries, and this policy should be a nonstarter.
In addition to the problems with the policy itself, once again the administration has let the clock wind down too far. The MFN rule has not been previously proposed, so technically a proposed rule must be issued before a final rule. But short on time, the administration is expected to issue an interim final rule (IFR) in an attempt again to sidestep the rulemaking process. As luck would have it, Bosch also has an explainer on IFRs and why this one is likely to run into legal challenges.
To summarize, having run out of time the administration is trying to force a number of significant regulatory efforts through at the last minute, bypassing the established rulemaking process. It’s an ironic end for an administration that touts deregulatory actions among its top accomplishments.
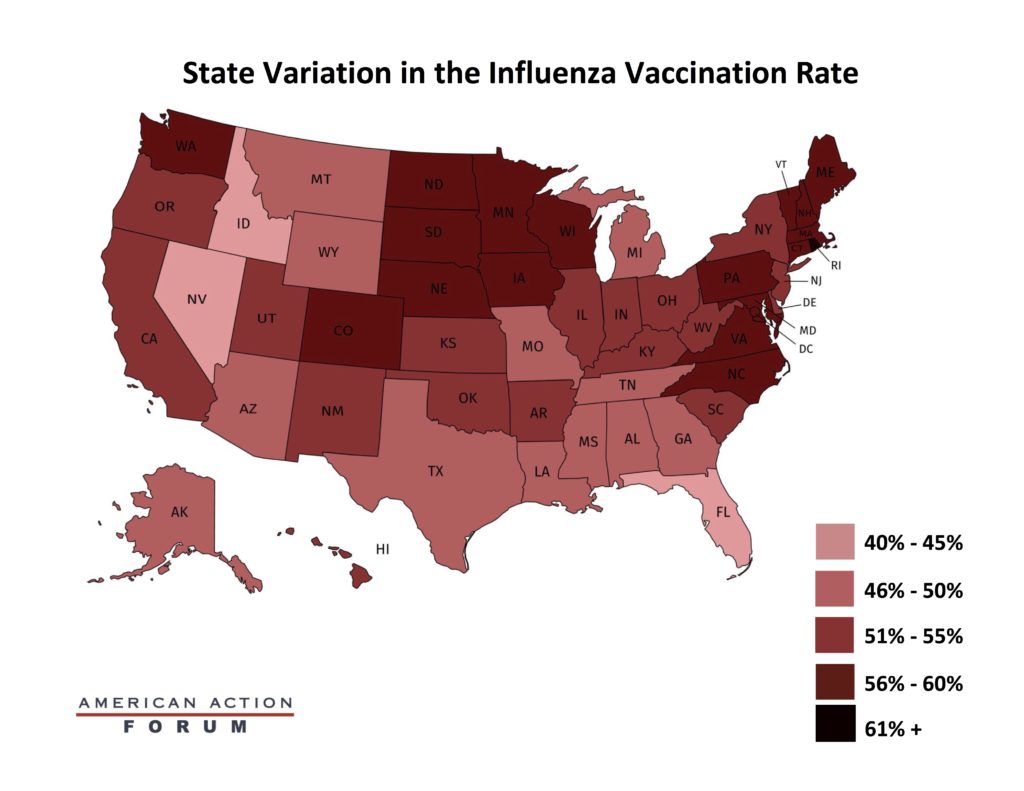
Chart Review: Flu Vaccination Rates
Julia Demeester, Health Care Policy Intern
The successful development of a COVID-19 vaccine is only half of the battle; for a vaccine to be successful, enough people must receive it. The flu vaccine provides a rough indicator of both how many people accept vaccines each year and how well states do in promoting immunization. Despite the general accessibility of the annual vaccine—most can receive it for free—the rate of vaccination last year was just 52 percent of individuals 6 months and older. As the map below shows, rates were the highest in the Northeast and the lowest in the West. State variation of the annual flu vaccine could indicate where a COVID-19 vaccine will be implemented widely and where it will struggle to reach sufficient levels of immunization within the population. The varying rates of flu vaccine uptake across the country can therefore inform where targeted efforts may be necessary for encouraging a COVID-19 vaccine. A report released by the Kaiser Family Foundation states that to achieve sufficient levels of immunity against the coronavirus, most Americans will need to be vaccinated, and so variation in COVID-19 vaccination rates could drastically impact efforts to control the pandemic. The federal government has stated that it will ensure the COVID-19 vaccine is provided free of charge to all, even uninsured individuals. Universal access to the vaccine is likely to boost the vaccination rate.
Data source: Kaiser Family Foundation
From Team Health
The Impact of a Most Favored Nation Drug Price Rulemaking on Innovation – Director of Health Care Policy Christopher Holt and Director of Human Welfare Policy Tara O’Neill Hayes
The administration’s expected rule pegging Medicare Part B prices to those in other countries will slash the funding available for research and development.
More Frickin Nonsense (MFN) – AAF President Douglas Holtz-Eakin
The policy of pegging drug prices to those paid in other countries is a bad one, and the administration’s approach of implementing it through an interim final rule is no better.
Policy Interventions to Mitigate Individual-Level Risk Factors that Contribute to Chronic Disease – Tara O’Neill Hayes and Serena Gillian
A multitude of factors contribute to an individual’s risk of chronic disease, including not just lifestyle and family history but also education and income.
Worth a Look
The Wall Street Journal: Opioid Deaths in Canada Were Falling, Then Came Coronavirus
Modern Healthcare: FDA allows 1st rapid virus test that gives results at home