Insight
August 3, 2023
Addressing the High Costs of Air Ambulance Services
Executive Summary
- Over 550,000 patients use air ambulance services annually in the United States, but often these trips represent a significant economic burden with a per-trip median cost of $36,000.
- The air ambulance industry’s exorbitant costs are likely the result of its significant concentration, as there are few competitors in the market.
- Congressional or state legislation may be able to promote competition via antitrust laws and regulation of natural monopolies in the air ambulance market, but policymakers must have a better handle on the specific cost drivers involved before acting, which they can gain through more rigorous data collection.
Introduction
Air ambulances, which are specially equipped aircraft used to transport individuals to a hospital, are a critical piece of transportation infrastructure for the health care industry that save thousands of lives every year. Air ambulances are most frequently deployed for rural patients who need to be transported to hospitals quickly or for patients who are in need of rapid emergency care. Yet many of these patients are often financially unprepared to pay the large bills that show up in their mail following a trip to the emergency room in an air ambulance. The median cost for an air ambulance trip is $36,000 – about $23,000– $30,000 more expensive than the operating cost of an air ambulance flight, and[1] over 36 times more expensive than the $950 average cost of a basic life-support ground ambulance trip.[2]
This stark difference between operating costs and costs consumers face from an air ambulance trip can be accounted for by the high degree of market concentration by only three firms in the market (owning 73 percent of air ambulance helicopters), the lack of incentives for insurance companies to engage with air ambulance companies, and the barriers to entry for new firms.[3] Coupling these problems with a lack of agency for patients who need this care, firms have the ability to inflate prices to exorbitantly high rates, often much higher than the operating cost.
Under the Airline Deregulation Act of 1978, the government, at any level, lacks the authority to craft a policy response to the air ambulance market distortion. Additionally, there remains limited data available about which specific aspects of a given air ambulance operation truly drive the costs upwards. In order to better address this issue, policymakers need both a greater understanding of these details – which some recent legislation seeks to address – and greater authority to act on such findings in an appropriate manner.
Background
In the 1960s, R Adams Cowley, a trauma doctor in Maryland, hypothesized that his patients had a pivotal window of opportunity to receive life-saving trauma care; he eventually dubbed this window of opportunity the “Golden Hour.” According to the Golden Hour principle, the first 60 minutes following a trauma-inducing event is critical for receiving healthcare. Dr. Cowley operated under this pretext and saw great success with the care of his patients. He worked alongside Maryland State Police to have patients brought to the shock trauma unit of the hospital via military helicopter, and thus in 1969, the air ambulance was born. Over the decades, air ambulances have become more popular, allowing patients (especially those in rural areas) to get to a hospital faster.
The Current Situation
Today, over 550,000 American patients use air ambulances annually, making it a critical aspect of healthcare infrastructure, especially for more rural areas of the country. Yet many Americans are unaware of the cost of using an air ambulance. The median price for an air ambulance trip is $36,000. For context, the average cost of operating an air ambulance flight (according to air ambulance providers) is between $6,000–$13,000.[4] Why such a large discrepancy between the operating cost and the cost consumers pay? The answer: Regular market forces are not at play.
In an industry with normal market forces, prices and quantities of the goods supplied are dictated by the equilibrium between demand and supply. Therefore, the quantity demanded curve is negatively sloped as people buy less as the price increases (Figure 1). But in the air ambulance industry, the demand curve takes the shape of a vertical line (Figure 2). The quantity demanded stays the same, unaffected by price of the ambulance service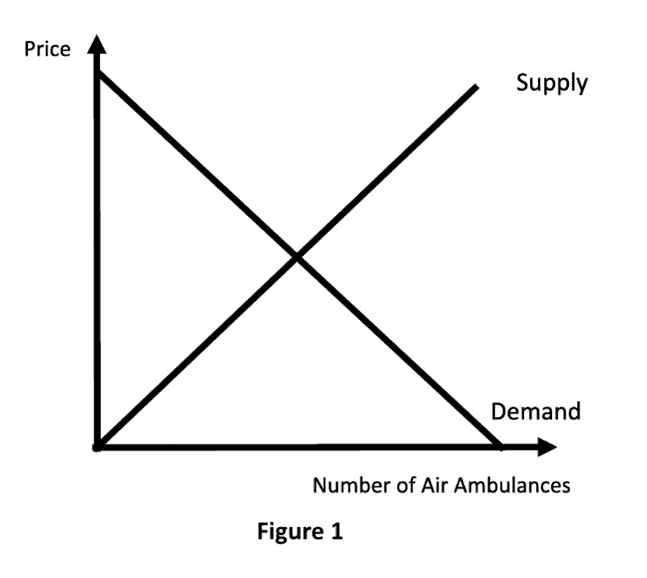
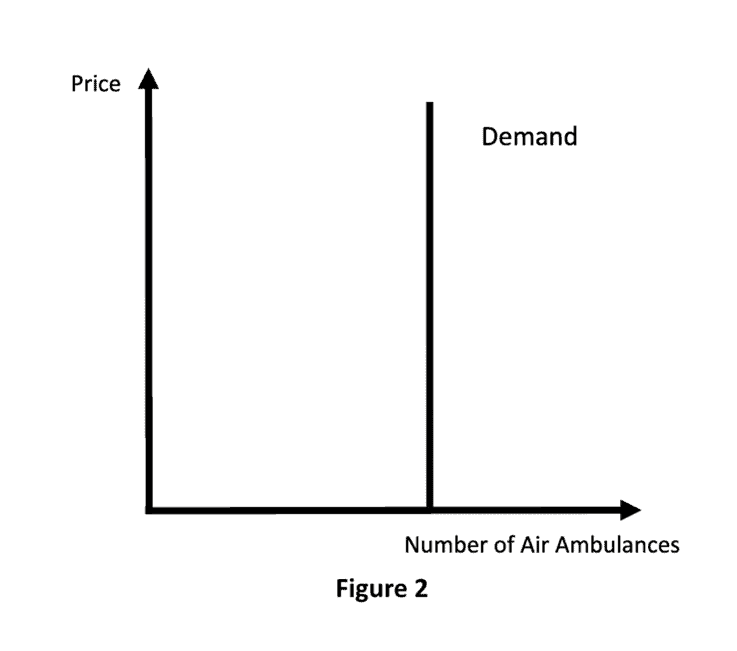 This vertical demand curve of the air ambulance industry can be explained by a few factors: Primarily, taking an air ambulance is often a matter of life or death, so patients are willing to pay whatever price is necessary for the service. What is more, in many instances where an air ambulance is needed, the patient lacks the agency to actually make the decision between an air ambulance or a regular ambulance, and thus must leave the decision to a medical professional.
This vertical demand curve of the air ambulance industry can be explained by a few factors: Primarily, taking an air ambulance is often a matter of life or death, so patients are willing to pay whatever price is necessary for the service. What is more, in many instances where an air ambulance is needed, the patient lacks the agency to actually make the decision between an air ambulance or a regular ambulance, and thus must leave the decision to a medical professional.
Is the Golden Hour principle necessarily the correct framework for medical care, and does it create overreliance on air ambulances? Several studies call into the question whether or not the Golden Hour is, in fact, the end-all-be-all in these situations. For instance, one study has concluded that a 90-minute window is comparable to a 60-minute window. Therefore, in adhering to an outdated standard, patients may take an air ambulance they do not need, potentially incurring tens of thousands of dollars in unnecessary charges.
Another important question is how insurance factors into the equation. It appears that there are few coverage options for air ambulance transports: “One large [air ambulance] company reported that it contracted with less than 1 percent of the 1,000 private insurers it works with per year.” That is likely a result of the fact that insurance companies lack an incentive to create plans that cover air ambulance trips, principally because the industry is so anomalous. Insurance companies would rather keep premiums low and cover more common medical expenses.
While high premiums associated with air ambulances may be seen as an incentive for more firms to enter the market, the high barriers to entry prevent competition in the industry. The Government Accountability Office notes that 73 percent of air ambulance helicopters are owned by just three firms.[5] An important question to consider is the geographical distribution of the three largest firms in the market. As demonstrated by these firms‘ self-reported maps of helicopter locations, it is apparent that there is a large overlap between their operating areas. Therefore, geography does not seem to be a large factor in the observable competition issues.
Multiple states have recognized these market failures and attempted to implement policy responses such as billing guidelines[6] as a result. These attempts have been largely unsuccessful, however, as air ambulance providers have successfully argued in court that they are technically airlines and therefore states lack authority to regulate them under the 1978 Airline Deregulation Act. While the law has allowed the United States to foster a largely successful airline industry, it also led (perhaps unintentionally) to deregulation of the air ambulance industry – despite its exceptionally flawed market structure. Congress and state governments alike thus currently lack the authority to implement corrective measures to address the market forces in play in this specific industry.
Potential Solutions
Properly understood, the failure of the air ambulance industry to enjoy normal market conditions is a medical issue, not an airlines issue. One solution for lawmakers to consider is to amend the Airline Deregulation Act of 1978 with language that excludes air ambulances from their current regulatory immunity. This would allow both state and federal governments greater leeway in crafting targeted responses to help correct this market failure. Before policymakers go down that road, however, it is important to get a clearer picture of the specific factors driving costs upward.
In recent years, several pieces of legislation have been enacted at the federal level to address this issue. Section 418 of the 2018 Federal Aviation Administration (FAA) Reauthorization Act requires the secretary of Transportation and the secretary of Health and Human Services to establish a committee that will “make recommendations with respect to [the] disclosure of charges and fees for air ambulance services and insurance coverage, consumer protection and enforcement authorities of both the Department of Transportation and State authorities, and the prevention of balance billing to consumers.”
The Consolidated Appropriations Act of 2021 addresses the high cost of air ambulances in a few ways. Primarily, it establishes that only the in-network cost-sharing amount is mandatory for individuals covered by employer-sponsored or commercial plans when it comes to out-of-network emergency care services such as air ambulance transports. Additionally, the law creates a separate resolution process for resolving conflicts between service providers and insurance plans and issuers.[7] The law also addresses air ambulances’ data collection. The law mandates the increase of data collection pertaining to the number and location of air bases, the reasons for denied claims, the number and type of aircraft used as air ambulances, and the costs of flights.
Whether these two pieces of legislation will make an impact on prices remains to be seen. Indeed, the lack of transparent air ambulance cost data is a complicating factor. While there is a general understanding on the average total cost of an air ambulance transport, the data on the cost of specific items are often far less clear. Until there is more information on the components of the total cost, it will be difficult to ascertain which aspects of an air ambulance operation require further attention and scrutiny. Ultimately, the data gathered under these pieces of legislation should help to better inform state and federal regulatory efforts.
Conclusion
While the use of air ambulances continues to increase, it still remains an anomalous practice. The 550,000 U.S. patients who use these air ambulances per year are often stuck with a shockingly high price tag. The air ambulance industry’s dense market concentration and high barriers to entry will only perpetuate high costs for these transports. The complex issue of air ambulances is an odd case where government regulation might be able to promote competition, but until policymakers have a better handle on the specific cost drivers involved and the ability to meaningfully address them, the high price many consumers pay will remain on auto-pilot.
[1] See page 16 of the document
[2] See page 7 of the document
[3] See page 2 of the GAO document
[4] See page 16
[5] See page 2 of https://www.gao.gov/assets/gao-17-637.pdf
[6] See “Table 2” on pg 20
[7] See Section 105 of the Act










