Research
November 10, 2016
Prospects for Care Coordination for Children with Medical Complexity
Executive Summary
- While most children covered by Medicaid require only routine and inexpensive medical services, some complex cases require considerable medical coordination and significant resources.
- Coordinating care between medical facilities and employing capitated payments, shared savings models, or other incentive-based payments could improve medical outcomes and save both federal and state Medicaid dollars.
- Proposed changes to the care coordination of medically complex children covered by Medicaid could save as much as $13 to $16 billion over the first 10 years of implementation, and has the potential to save more in future years.
Over 30 million children are covered by Medicaid programs in the United States. While the vast majority of these children are relatively healthy and require only routine, low-cost health care, a small percentage have extremely serious, highly complex, and/or multiple diseases requiring substantial amounts of health care. This group, sometimes referred to as Medically Complex Children (MCC), or Children with Medical Complexity (CMC) by various government agencies, comprise over 1.8 million children, or an estimated 6.5 percent of Medicaid-enrolled children as of 2008, yet account for approximately 40 percent of Medicaid spending on children’s health care.[i]
With such a large amount of spending in a concentrated population, it’s reasonable to think that a reform of care and/or payment systems for care of this population might result in significant savings without adversely affecting care, and perhaps even while improving it. In addition, these patients often require multiple hospitalizations and care from multiple physician specialists and clinics, often located in multiple states. These factors—particularly care providers from multiple states—are not circumstances Medicaid was designed to handle.
Proposals have been put forward to establish a different system for providing and paying for care of CMC patients. The idea is to have a children’s hospital, or another similar entity, manage care for each CMC patient as the patient’s “medical home.” That medical home would provide much of the care for the patient, and also arrange, coordinate, and pay for care provided by other entities, including physicians and specialty facilities that might be located in a different state. The state Medicaid program would then pay only the patient’s medical home for care of that patient; those funds would be used by the medical home to pay whatever other care providers became involved, including those in different states, if any. In some versions of the concept, the state Medicaid program could calculate that payment on a capitated monthly basis—that is, paying the medical home a fixed amount regardless of the type or amount of care required—but other payment models would also be permitted.
On Capitol Hill, the question is, as always, will this save money? Here we will review some reasons why this sort of plan might be expected to save money, a previous study that attempts to estimate the potential savings, and what details of implementation might affect what savings can be achieved. We find that in a relatively optimistic scenario, annual savings might be as high as 3.8 percent of annual spending on the CMC patient population, or up to $6 billion annually by 2027, amounting to a total of $13 to $16 billion in the first 10 years of program implementation.[ii]
Why Might Care Coordination for Medically Complex Children Save Money?
“Children with Medical Complexity” are defined as those who satisfy the criteria for Clinic Risk Groups (CRGs) 5b-9. That includes those with a significant lifelong chronic disease (CRG 5b), significant chronic disease in multiple organ systems (CRG 6), dominant chronic disease in three or more organ system (CRG 7), dominant or metastatic malignancy (CRG 8), or a catastrophic condition (CRG 9).
Like anyone with a complex disease or multiple diseases, children with complex medical conditions require the services of a variety of health care providers, including hospitals, outpatient clinics, emergency departments, and multiple physician specialists, not to mention laboratory and imaging facilities. In a fractured fee-for-service system, there are many foregone opportunities to achieve efficiency and avoid duplication. With care coordination, some efficiencies can be achieved. For example, with proper outpatient monitoring, the number of emergency visits and hospitalizations may be reduced. In addition, patients with complex conditions often receive treatment from multiple individual providers, including multiple physician specialists, and nonphysician providers such as nurse practitioners, physical therapist, and many others. When treating the same patient, it is important to make sure that all these providers have access to current information, and communicate with each other to make sure their efforts are complementary rather than duplicative – or worse, contradictory. The result might be reduced spending in some categories, such as emergency visits and inpatient stays, but increased spending in other categories, such as outpatient tests, office visits, prescriptions drugs, home health, and other treatments that prevent adverse episodes. Even if spending on outpatient procedures and prescription drugs increases as a result, total spending may be reduced, and patient well-being may be enhanced as well. If care is coordinated through a single entity, incentives can be better aligned with these factors.
Furthermore, in the case of relatively rare diseases, the best specialist might be in another state. Medicaid is a state-based program, and obtaining coverage for out-of-state care can be difficult and expensive, and the process can induce delays. However, if a single entity is paid to coordinate care for the Medicaid-eligible child, and can pay other providers, including out-of-state providers, directly without enrolling those providers in their own state’s Medicaid program, these problems could be avoided.
Of course, the coordination of care is itself a service that is costly to provide. The question to be asked is not only “would coordination reduce spending on health care itself?” but “would coordination reduce spending on health care by more than enough to cover the cost of coordination?” If not, would the improvement in patient well-being, if any, be worth the additional cost on its own merits?
Attempting to Measure the Savings
Predicting the savings from a nationwide program to implement care coordination through a medical home for the CMC Medicaid population is difficult, since no program has ever attempted to do precisely that. While there are good reasons to believe that savings are possible, the precise level of savings is somewhat speculative.
The best that can be done under these circumstances is to find instances in which something similar to the current proposal has been implemented, see what happened in those instances and compare it to what is proposed now. A group of researchers at Dobson DaVanzo & Associates (DDA)[iii] found eleven programs which implemented coordinated care programs for CMC patients or other pediatric patients with serious or complex medical histories.[iv] Prior studies of these programs found varying levels of reductions in utilization and/or health care costs, either before and after the programs were implemented, or when comparing patients enrolled in these coordination programs to otherwise similar patients who were not enrolled. Using these studies, they estimated utilization changes in various categories as follows (with the share of overall Medicaid spending shown for convenience):
|
Spending Category |
Estimated
Utilization Change |
Share of Overall Medicaid Spending |
| Inpatient facility | ‒40% | 47% |
| Outpatient facility | +10% | 31% |
| Emergency Room | ‒20% | 3% |
| Primary Care Providers | +30% | 2% |
| Prescription Drugs | +10% | 14% |
| Other | N/A | 3% |
Using those studies to estimate changes in various spending categories, they then applied those changes to estimates of the overall Medicaid spending on the CMC population using 2011 data. Under the assumption that current Medicaid spending is based on uncoordinated fee-for-service care, they estimate that the total savings would be in the range of 0.9 percent to 3.8 percent, or $6 billion to $26 billion, over ten years.
This is a good first step, but it is limited due to the data available to the researchers. None of the programs they use for comparison use precisely the targeted population, and the programs were in fact established for other reasons. At the same time, a comparison to a fee-for-service Medicaid program no longer tells the full story, as Medicaid managed care has been implemented more widely since the data used in the DDA study were taken.
In a critique of the DDA study, Steve Lieberman[v] points out that if legislation were to pass implementing the proposed program, it would take time for the Centers for Medicare and Medicaid Services to enact regulations to implement the program, and afterwards it would take additional time for children’s hospitals and other prospective medical homes to develop plans to implement the program, establish provider networks and other relationships, and so on. On this basis, Lieberman objects to the 10-year savings total projected by DDA. By keeping the start-up costs where they are and pushing the start of savings back two years, Lieberman calculates that in the ten years after legislation passes, the five years of remaining savings will not fully offset the start-up costs.
While this criticism has some validity, it reflects only the timing of savings, not whether they will occur. For a program that is expected to exist for a long time, it would be short-sighted to reject it due to artifacts caused by the construction of a ten-year budget window.
Lieberman also points out that the DDA study does not include any estimates of effects on spending for long-term and social support (LTSS) services.[vi]It would be good to have a study that took LTSS into account. That could either increase or decrease the savings. It is not appropriate to assume, without investigation, that it would cancel out the savings.
Lieberman’s third criticism is that Medicaid managed care may have already produced, or could produce, some of the savings that the CMC medical home concept could produce. This is framed as a criticism that “savings are overstated.” It could just as easily be regarded as confirmation that care coordination can save money, but that not all the savings have been achieved yet.
Incentives and Capitated Payments
One possible version of the CMC medical home concept that is not accounted for in any of the published estimates is the possibility that the program entails a switch from a fee-for-service payment system to capitated payments to a single entity, and the change in incentives effectuated by that switch is key to determining whether, and to what extent, savings are achieved.
Capitated payments are the key component of Medicare Part D (where they have achieved substantial savings relative to projected costs[vii]), and of Medicare Advantage and many Medicaid managed care programs. The key factor in any capitated payment system is calculating the capitated payment for each patient. It is tempting to think that one can “guarantee” savings by setting the payment to be lower than the patient’s expected fee-for-service spending; however, that is only partly true, and it sets a cap on the savings as well.
If the capitated payments are set too low, prospective medical homes will not want to participate, since they will lose money (on average) for every patient they accept. If the program is not mandatory, patients will therefore not be enrolled, will remain in a fee-for-service program, and no savings will be achieved, despite the aggressively low capitation rate. If the program is mandatory for patients but medical homes do not come forward, the result will be disastrous, as patients will have no providers from whom to obtain care.
On the other hand, if capitated payments are too high, care will be easily available but savings will not be achieved.
There are “in-between” possibilities as well: if capitation rates are just a little bit low, but not low enough to keep medical homes from participating, they will participate but will be forced to restrict care for patients. If capitation rates depend on diagnosis (as they must), care must be taken to ensure that rates are not subject to manipulation based on small (but medically defensible) changes in diagnoses.
It should be clear that the method of calculating capitation rates is critical, and any estimate of savings based solely on existing fee-for-service payments without considering the proposed formula for capitated payments is, at best, a good starting point for estimating savings but not the endpoint.
Actual Savings Depends on the Actual Payment System
A recently considered discussion draft of proposed legislation, named the “Advancing Care for Exceptional Kids Act” or the “ACE Kids Act”[viii] does not actually require capitated payments. It allows capitated payments, but specifies that they are not required, and also allows “shared savings models, pay-for-performance models, contingency awards dependent on reducing utilization of emergency departments, or other incentive-based approaches.” It appears that the decision is to be made by each state, not each medical home, although that is not entirely clear.
Ranging Plausible Savings
Without more clearly specifying the payment model, a precise estimate of savings is not possible. However, we can provide plausible upper and lower bounds on the savings that might be achieved, as well as a “middle ground” estimate assuming a reasonable payment model.
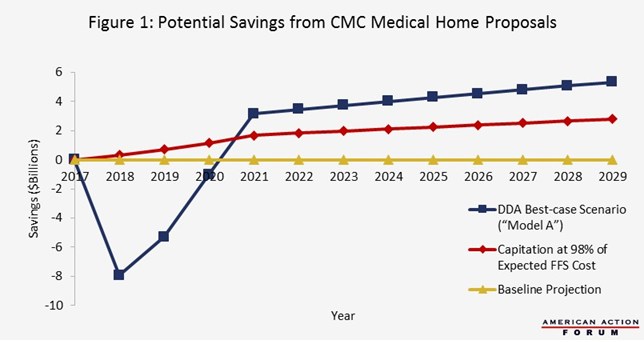
For a best-case scenario, we use the DDA study’s “Model A” (Targeted Efficiencies). This model assumes a fee-for-service environment, in which care coordination is a service that CMC medical homes are explicitly paid to provide. Their conclusion is that while payments for care coordination (and certain others classes of services) will increase, total payments for other classes of services will decrease by more than enough to make up for the difference, resulting in an overall savings of 3.8 percent of baseline CMC spending in the final steady-state, which amounts to approximately $6 billion dollars per year by 2027. In the first three years, the model predicts an increase in spending (shown in Figure 1 as negative savings), under the assumption that care coordination costs more in the startup years, and achieves less savings until systems mature. This is consistent with other experiences with new systems. The initial investment pays for itself by approximately year 7 of the program (2024 in the Figure) and savings continue to accrue thereafter.
For the “middle” case, we assume that a capitated payment system is set up, with the effect of setting payments at 98 percent of the expected payments under the baseline fee-for-service system. Clearly, this would have to be set individually for each patient based on that patient’s diagnosis codes and possibly demographic features, in a manner similar to that used for risk adjustment in the Medicare Advantage and Medicare Part D programs.[ix] We also assume that a phase-in period is required, in which it takes approximately four years to enroll all CMC patients in such programs. This scenario involves no increase in spending at the beginning, and achieves savings in excess of $3 billion per year by 2027, increasing thereafter.
For the worst-case scenario, we note that if no states choose to participate in the program, or if states choose to participate but no prospective medical homes enroll, the projected spending will be the same as current baseline projections. The result in either case is, of course, zero savings.[x]
These three scenarios are illustrated in Figure 1. The scenarios assume that the legislation is passed in 2017 and implementation begins in 2018. If passage is delayed or implementation takes longer to begin, appropriate adjustments will have to be made. The overall pattern will be the same, but the dollar figures will be different since projections of baseline Medicaid spending rise with time, in part due to a growing population. Note that these projections include spending on health care only; they do not include the cost to federal and state governments of writing and publishing regulations to implement the program. We expect that the cost of writing regulations will be small relative to the health care costs involved.
Conclusion
Care coordination for Children with Medical Complexity is a serious problem that deserves serious consideration, especially in the context of Medicaid, where fee-for-service fragmentation and state boundaries present serious problem that lead not just to unnecessarily high costs, but to unnecessary adverse health consequences for children.
A proposal to encourage care coordination through a children’s hospital or some similar qualified institution shows promise, both in terms of rationalizing care delivery and improving health and quality of life for affected children and their families, and also in terms of saving money. Available data show only part of the picture, and do not seem to allow for accurate estimates of incentive effects. Currently proposed legislation is quite specific as to the type of care coordination envisioned, but not specific as to the method of calculating payments to providers.
A coordinated medical home model for medically complex children has the potential to save program dollars and to improve medical outcomes for complicated cases. Specifying a payment model that provides the desired degree of flexibility, while capping spending at some formula designed to approximate spending will be key to the success of a shift to a medical home model. Useful payment models may be found in other health care programs that already provide for risk-adjusted capitated payments, such as Medicare Advantage and Medicare Part D.
[i] Allen Dobson, Joan E. DaVanzo, Gregory Berger, Matt Shimer, Audrey El-Gamil, Kevin Reuter, Steven Heath, Nikolay Manolov, “Savings Estimate of a Legislative Proposal to Improve Care Coordination for Medically Complex Children within the Medicaid Program,” Dobson DaVanzo & Associates, October 17, 2013.
[ii] These estimates are for the first 10 years of implementation. The relationship between this and the standard CBO budget window depends on the amount of time between enacting the appropriate legislation and implementing it. If one assumes that implementation will take, say, two years after enactment, two years of savings will be pushed beyond the standard budget window.
[iii] Allen Dobson, Joan E. DaVanzo, Gregory Berger, Matt Shimer, Audrey El-Gamil, Kevin Reuter, Steven Heath, Nikolay Manolov, “Savings Estimate of a Legislative Proposal to Improve Care Coordination for Medically Complex Children within the Medicaid Program,” Dobson DaVanzo & Associates, October 17, 2013.
[iv] The eleven studies used by DDA are documented in the following ten publications (the Treo publication includes two):
Gordon, J.B., Colby, H.H., Bartelt, T., Jablonski, D., Krauthoefer, M.L., Havens, P. (2007), “ A tertiary care primary care partnership model for medically complex and fragile children and youth with special health care needs,” Archives of Pediatric Adolescent Medicine 161(10), 937-944.
Casey, P.H., Lyle, R.E., Bird, T.M., Robbins, J.M., Kuo, D.Z., Brown, C., et al. (2011), “Effect of hospital-based comprehensive care clinic on health costs for Medicaid-insured medically complex children,” Archives of Pediatric Adolescent Medicine 165(5), 392-398.
Treo Solutions. (2012, June), Performance analysis: Healthcare utilization of CCNC-enrolled population 2007-2010.
Peter, S., Chaney, G., Zappia, T., Van Veldhuisen, C., Pereira, S., Santamaria, N. (2011), “Care coordination for children with complex care needs significantly reduces hospital utilization,” Journal for Specialists in Pediatric Nursing 16(4), 305-312.
Klein, C., LaCoste, J. (2011, July), Children’s Healthcare Access Program 2010 Annual Report, SRA International, Inc.
Hawkins, M.R., Diehl-Svrjcek, B., Dunbar, L.J. (2006), “Caring for children with special healthcare needs in the managed care environment,” Lippincotts Case Management 11, 216-223.
Cohen, E., Lacombe-Duncan, A., Spalding, K., MacInnis, J., Nicholas, D., Narayanan, U., Gordon, M., Margolis, I., Friedman, J.N. (2012), “Integrated complex care coordination for children with medical complexity: A mixed-methods evaluation of tertiary care-community collaboration,” BMC Health Services Research 12:366.
Klitzner, T.S., Rabbitt, L.A., Chang, R.K. (2010), “Benefits of care coordination for children with complex disease: a pilot medical home project in a resident teaching clinic,” Journal of Pediatrics 156(6), 1006-1010.
Fiks, A.G., Mayne, S., Localio, A.R., Alessandrini, E.A., Guevara, J.P. (2012), “Shared decision-making and health care expenditures among children with special health care needs,” Pediatrics 129(1), 99-107.
Complex Chronic Pediatric Center, St. Joseph’s Children’s Hospital, “Cost effectiveness study: St. Joseph’s Children’s Hospital Baycare Health System,” (Unpublished).
[v] Steve Lieberman, “Is H.R. 546 Likely to Result in Federal Medical Savings?” Lieberman Consulting, Inc., September 8, 2015.
[vi] It is also true that neither the DDA study nor the Lieberman critique discuss the effects on public education spending or parks and recreation services, both of which are utilized by the CMC population.
[vii] Douglas Holtz-Eakin and Robert Book, “Competition and the Medicare Part D Program,” American Action Forum, September 11, 2013, at https://www.americanactionforum.org/research/competition-and-the-medicare-part-d-program.
[viii] As of this writing, the bill has not been formally introduced, but was the subject of a hearing in the House Energy and Commerce Committee on July 7, 2016. The proposed bill text is available at http://docs.house.gov/meetings/IF/IF14/20160707/105165/BILLS-114pih-DiscussionDraft.pdf.
[ix] Robert Book, “Primer: Medicare Risk Adjustment,” American Action Forum, February 11, 2015, at https://www.americanactionforum.org/research/primer-medicare-risk-adjustment.
[x] We are assuming here that the cost of writing regulations is negligible with respect to the total spending on CMC patient care.