Weekly Checkup
July 20, 2018
Clearing Obstacles to Medicare Innovation
It’s no secret that legislation and regulation frequently cause unintended downstream challenges. For example—as detailed in last week’s edition of the Weekly Checkup—the creation of Medicaid “best price” unintentionally undermined drug makers’ willingness to provide their medications at a discount for underinsured (and uninsured) patients, leading to the creation of the now-bloated 340B Drug Discount Program. Even well-intentioned and effective legislative efforts can cause problems for policymakers down the road. Policies aimed at today’s challenges can evolve into impediments to tomorrow’s innovation.
So it is with the myriad rules, regulations, and statutes that have accrued over time to mitigate corruption within Medicare’s fee-for-service payment system. In particular, the Stark Law has come under the microscope recently, as policymakers look to further transition Medicare to payment models that prioritize value rather than simply the number of procedures. (The Stark Law also has implications for value-based payment arrangements in the drug space as well—as detailed by AAF’s Tara O’Neill Hayes here). Last week Centers for Medicare and Medicaid Services Administrator Seema Verma singled out Stark as “one of the barriers around value-based care.”
Simply put, the Stark Law seeks to prevent physicians from referring patients to facilities or practices in which the referring physician or a close family member has a financial stake. While this prohibition made sense when it was passed, and the statute provides some safe harbors to allow for exceptions, these restrictions have made some of the innovative payment models currently being developed—as well as improved care coordination—legally problematic.
More people than just Administrator Verma are talking about the Stark Law. The House Ways and Means Committee held a hearing this week on “Modernizing Stark Law to Ensure the Successful Transition from Volume to Value in the Medicare Program,” in which Health and Human Services (HHS) Deputy Secretary Eric Hargan testified in more detail about the obstacles Stark erects to improving the Medicare program. And, in things you don’t see every day, former HHS Secretaries Tommy Thompson and Kathleen Sebelius co-authored an op-ed further elaborating on the impediment that Stark and other anti-kickback statutes are to innovation.
According to Administrator Verma, the Trump Administration is aiming to “have something out by the end of the year.” Perhaps, if the Thompson-Sebelius convergence is indicative, efforts to remove barriers to innovative payment policies could provide a rare opportunity for bipartisan cooperation on health care policy—and in an election year no less.
Chart Review
Tara O’Neill Hayes, Deputy Director of Health Care Policy
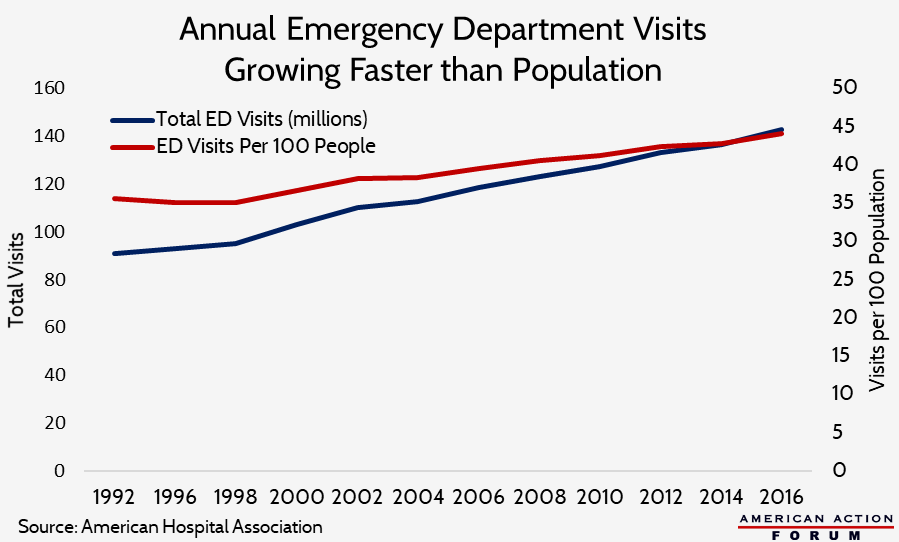
Americans’ use of emergency departments has been rising steadily for decades, and rising at a rate faster than our population growth, as shown in the chart below. This growth has occurred even as the number of emergency departments has declined, putting even greater stress on the remaining ones. As a result, hospitals struggle to use limited resources efficiently and ensure those patients with true emergencies are treated in a timely manner.
Worth a Look
Reuters: Swiss, German drugmakers join U.S. price freeze
Wall Street Journal: Health-Care Coverage Is Increasingly Determined by Where You Live