Weekly Checkup
March 6, 2020
CMMI and the Separation of Powers
Here at the Weekly Checkup, we spill an awful lot of ink on executive-branch rulemaking. The reason is that for years now, Congress’s inability to meaningfully legislate has functioned as a de facto capitulation to the executive branch. This dynamic has been true under both the Obama and Trump Administrations and regardless of which party controls either chamber. Section 3021 of the Affordable Care Act (ACA), which established the Center for Medicare and Medicaid Innovation (CMMI), is a particularly egregious example of Congress actively ceding authority to the executive branch. But there has been a clamor for Congress to claw back some of its constitutional authority over health care policy by placing some appropriate limitations on CMMI’s overbroad authority.
The ACA established CMMI for the purpose of testing “innovative payment and service delivery models to reduce program expenditures…while preserving or enhancing the quality of care.” Objectively there is value in this goal. But CMMI operates without any real checks and significantly expands the power of the executive branch. CMMI can rapidly scale up its demonstration projects to encompass the entire country if it deems them successful and can leave them in place indefinitely. In order to scale up the demos, the demos must either reduce spending without reducing the quality of care, or improve the quality of care without increasing spending, and they must not deny or limit the coverage or provision of any benefits. In practice, however, this determination is made by the Secretary of Health and Human Services. Effectively, then, CMMI allows the president to make wholesale changes to federal health care programs that would have required congressional action prior to the ACA. One recent example that has been widely discussed is the International Price Index (IPI) proposal that has been floated by the Trump Administration. In addition to being terrible policy, it’s the sort of policy change that could have only been implemented by Congress prior to the establishment of CMMI.
In theory, Congress can block CMMI initiatives, like the IPI, but of course that requires both chambers of Congress to pass legislation doing so—an increasingly high bar these days. An additional challenge relates to how the Congressional Budget Office (CBO) scores executive actions. If the administration proposes a rule, CBO calculates the fiscal impact and then automatically includes half the of the savings (or costs) in the baseline. As a result, if CBO determines a rule would reduce federal spending by $100 billion, then any congressional action blocking it would cost $50 billion. The administration doesn’t have to find the money to pay for the policy when finalizing the rule, but Congress has to pay for rolling it back. If the rule were finalized, Congress would have to scrape together the full $100 billion in estimated savings in order to repeal it.
I’ll go ahead and put my cards on the table. While I’m a health care policy wonk by day, when I really cut loose and let my hair down, my passion is separation of powers. Article I all the way. Obviously, my kids think I’m really cool. So, given my bias toward Congress taking up its constitutionally prescribed powers to make the laws, I’d be happy to see CMMI repealed altogether. But from a health-policy perspective, CMMI does provide some valuable tools, and repeal is unrealistic for a host of reasons. Republican lawmakers were at the forefront of efforts to at least place guardrails around CMMI’s authority during the Obama Administration, but unfettered power to implement your policy ideas is a powerful drug, and many had a change of heart when President Trump took over.
Still, hope springs eternal, and a bipartisan group of lawmakers recently introduced legislation aimed at “strengthening” CMMI, which is a polite way of saying they want to put some constraints on it. Among other guardrails it would implement, the “Strengthening Innovation in Medicare and Medicaid Act,” (H.R. 5741) would place time limits on CMMI’s models, limiting them to a duration of 5 years and restricting their scope to only the necessary number of participants to obtain a statistically valid sample. The legislation also seeks to make it easier for Congress to block problematic demonstrations, and removes an egregious (and likely unconstitutional) prohibition on judicial review of CMMI models. These seem like reasonable policies, but at a very minimum Congress should act legislatively to give itself a role in approving nationwide demonstrations that functionally supersede federal law.
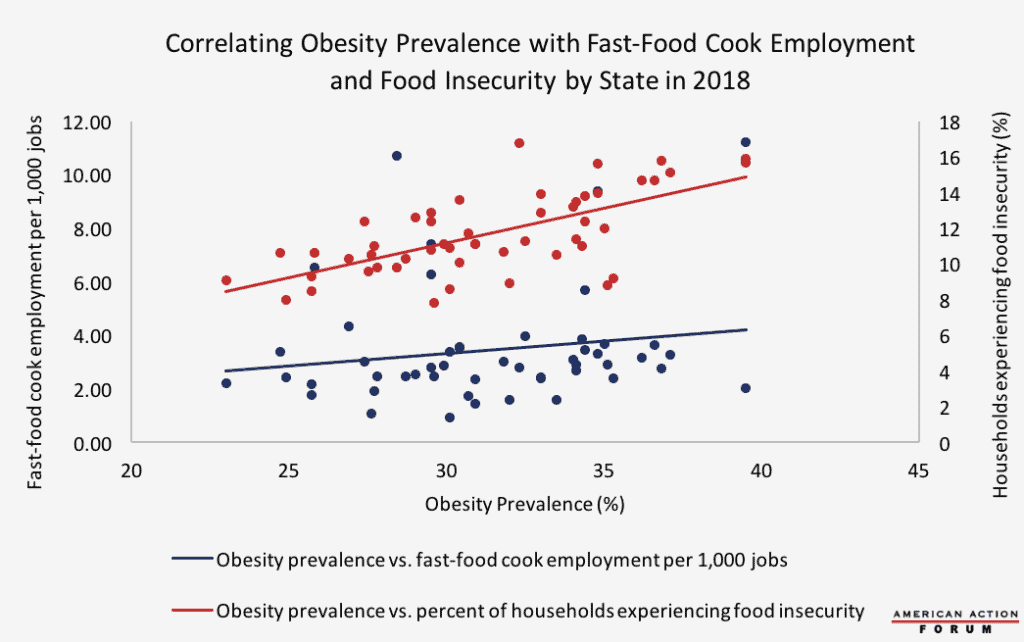
Chart Review: Obesity Prevalence, Food Insecurity, and Fast-Food Employment
Margaret Barnhorst, Health Care Policy Intern
The Centers for Disease Control and Prevention (CDC) recently published a study on obesity prevalence in the states. Colorado has the lowest obesity prevalence, at 23 percent, while Mississippi and West Virginia have the highest prevalence at 39.5 percent. Food insecurity could be one driver of obesity: A higher proportion of a state’s population that has low access to diverse and healthy food sources correlates relatively strongly with obesity (r=0.66). Yet fast food does not seem to be the primary substitute for a healthy diet, as the correlation between obesity and fast-food cook employment per state in 2018 (r=0.16) is much lower, as the chart below shows. This discrepancy may suggest that fast-food restaurants are not the main food source driving high obesity rates in food-insecure areas. Instead people may turn to convenience stores or mom-and-pop shops that have only limited food selection.
Data sources: CDC Behavioral Risk Factor Surveillance System, Bureau of Labor Statistics Occupational Employment Statistics Query System, U.S. Department of Agriculture Household Food Security in the U.S. in 2018
Note: Data from USDA Food Security report use average household food insecurity per state from 2016-2018. All other data are from 2018.
From Team Health
Understanding the Insulin Market – Director of Human Welfare Policy Tara O’Neill Hayes
While several factors have constrained the market for insulin, allowing prices to rise, new regulatory pathways will allow more competitors to enter the market in the coming years.
Worth a Look
Kaiser Health News: During A Pandemic, States’ Patchwork Of Crisis Strategies Could Mean Uneven Care
New York Times: Moderate Drinking Tied to Lower Levels of Alzheimer’s Brain Protein