Weekly Checkup
May 15, 2020
Grappling with COVID-19 in Long-term Care Facilities
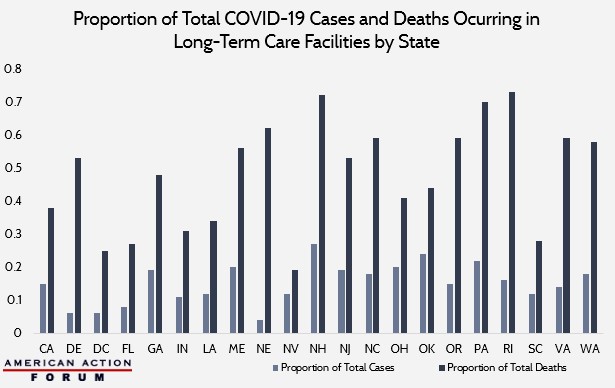
The Kaiser Family Foundation recently released research on state data and policy actions related to COVID-19, and within it are some notable revelations about the impact of the virus on long-term care facilities (LTCs). Out of the 33 states reporting data on COVID-19 in LTCs, the cases occurring in these facilities account for about 15 percent of total cases; Nebraska has the minimum at 4 percent, and New Hampshire has the maximum at 27 percent. For deaths, however, the proportion is far more troubling: 46 percent of all COVID-19 deaths occur in LTCs, ranging from Nevada at 19 percent to Rhode Island at a staggering 73 percent. The chart below illustrates these discrepancies.
Why are LTC residents dying at higher rates? There are a number of reasons, and while some obvious public health issues are contributing, we should not overlook the impact of regulation and policies, as well. The issues are tricky, however, as overregulation, underregulation, and inappropriate regulation have all contributed at different points.
Look to New York for examples of overregulation. Back in March, Governor Andrew Cuomo issued a mandate stating that nursing homes could not discriminate against residents who test positive for COVID-19. This required LTCs to readmit some back into their facilities, despite evidence coming out of Washington state in early March and long-term care organizations speaking out against such a policy. While Cuomo reversed the mandate last week, it remained in place during the most severe period of cases in New York. Of note, New York has yet to release its proportion of total deaths occurring in LTCs, although its total proportion of COVID-19 cases is at 20 percent.
Additionally, while Cuomo’s restrictions on LTC visitation were well-intentioned, they were too all-encompassing. The restrictions barred people such as ombudsmen—who are critical advocates for residents against maladministration—from entering LTCs, hampering oversight of nursing home practices.
Looking beyond New York, there may also be some link between Certificate-of-Need (CON) laws and poor LTC quality. Evidence suggests that the presence of state CON laws for nursing homes is linked to lower access, lower quality, and distorted (typically decreased) nursing home size. The link between CON laws and COVID-19 deaths isn’t clear-cut: Nevada has CON laws, while New Hampshire doesn’t. But given the link between lower quality and these laws, they are worth examining critically.
To see the problem of underregulation, one should look no further than inadequate staff-to-resident ratios. According to data from the Long-Term Care Community Coalition (LTCCC), the average LTC provides 3.37 hours of care per resident per day (HPRD), split between registered nurses (RN), certified nurse’s aides, and other qualified health care providers. This number falls well short of the recommended HPRD of 4.1, which is backed by independent research. Additionally, it is recommended that 30 percent of this 4.1 HPRD be provided by an RN, but the data from the LTCCC report that, on average, only about 13 percent comes from RNs. These numbers indicate that fewer nursing staff are required to care for more patients in a given day, leading to both inadequate care per patient and increased potential for disease transmission. Tailoring state-level legislation to decrease the number of patients any RN has at one time while increasing mandatory total care for each patient per day would help improve their overall well-being while diminishing cross-contamination.
Beyond the regulatory environment, LTCs are already set up for some degree of failure due to the frailty of the aging residents and the fact that they largely reside indoors. There is very little evidence to support large scale, outdoor transmission of COVID-19. Most of the spread researchers have been able to track has occurred indoors. Social distancing protocols forcing people into their homes exacerbates the problem for the elderly residing in LTCs. Not only are they tightly confined into their own spaces, but every nurse and visitor seeing them provides an opportunity for the virus to spread. Even with restrictions on visitation, clearly this is not problem that can be completely resolved.
As the examples above show, the solution to higher deaths in LTCs is neither regulating everything into tyrannical order nor some Wild West free-for-all. The goal should be to implement the right regulation, in the right place, at the right time.
From Team Health
Health Policy Provisions in the HEROES Act – Christopher Holt, Director of Health Care Policy
The health provisions in House Democrats’ proposal for a fourth coronavirus response bill can be divided into additional money for current programs and new or altered programs.
The Outsized Impact of the Coronavirus Pandemic on Minority Communities – Tara O’Neill Hayes, Director of Human Welfare Policy
Racial and ethnic minorities in the United States will feel disproportionately the health and economic impacts of the COVID-19 pandemic.
Worth a Look
New York Times: Coronavirus May Pose a New Risk to Younger Patients: Strokes
Health Affairs: Strong Social Distancing Measures In The United States Reduced The COVID-19 Growth Rate