Weekly Checkup
October 4, 2019
The President’s Plan for Medicare
This week President Trump rolled out a new executive order (EO) aimed at improving the Medicare program, and Medicare Advantage (MA) in particular. The White House framed the EO in contrast to Democrats’ embrace of “Medicare for All,” contending their proposals would harm seniors and reduce their benefits, while President Trump would protect seniors’ health care and defend Medicare. Like most EOs, this week’s action doesn’t actually do all that much itself. But it does start a process that could result in some noteworthy changes to Medicare down the road. Let’s look at some of what the administration is considering.
The overall theme of the EO is one of positioning MA to compete better with traditional fee-for-service (FFS) Medicare. To this end, the EO directs the Secretary of Health and Human Services (HHS) to do several things specifically for MA. The Secretary must propose regulations aimed at making Medicare Medical Savings Accounts available to more beneficiaries, and the Secretary must promote new payment models that would allow enrollees to receive direct financial benefits, potentially even cash payments, from savings achieved by plans. The EO also directs the Secretary to propose adjustments in network adequacy requirements, particularly in areas where certificate-of-need laws could restrict the availability of providers, in part by potentially allowing telehealth services to be used in meeting network requirements.
Other provisions address the entire Medicare program or FFS specifically. For example, the EO directs the Secretary to report within 180 days on ways to inject “true market-based pricing in the FFS Medicare program” and better align FFS payments with those of MA and the commercial market. Spoiler alert: The report will likely recommend congressional legislation, as existing statutes have a lot to say about what FFS pays. It’s not clear how this effort would fit with the broader effort to improve MA’s relative position verses FFS, as FFS is notorious for paying less than the commercial market. Aligning FFS with the market could mean increasing FFS payments to physicians, putting it in a better position relative to MA. The EO also includes provisions aimed at increasing the speed with which Medicare starts covering new therapies and medical technologies once they’ve been approved by the Food and Drug Administration, as this lag time has long frustrated drug and device manufacturers as well as patients. Further, the EO directs the Secretary to adjust reimbursements such that physicians are paid for time spent with patients and not just procedures performed.
Additional provisions seek to equalize reimbursements for similar treatments. The Secretary is directed to undertake rulemaking related to site-neutral payments—currently Medicare pays more or less for certain procedures depending on the type of care setting in which the service is received. The EO also targets equalizing payments for services regardless of the type of provider who performs them. In other words, if a nurse practitioner can perform a procedure under state laws, perhaps Medicare shouldn’t pay more when a doctor does it. Whether equalizing these payments would lead to all providers being reimbursed at the higher level, lowest level, or somewhere in between is not addressed. And, of course, there is the normal language about minimizing waste, fraud and abuse.
While the EO will have little immediate impact on the Medicare program, it certainly gives the HHS Secretary a full agenda of rulemaking. Some of the changes could be quite significant, though much will depend on the proposed regulations.
Chart Review
Andrew Strohman, Health Care Data Analyst
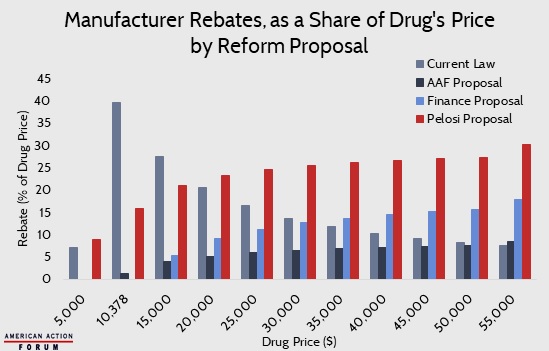
AAF’s Tara O’Neill Hayes recently published an Insight comparing three proposals to reform Medicare Part D and lower prescription drug costs. These proposals come from AAF, the Senate Finance Committee, and Speaker Pelosi. All three proposals aim to, among other things, increase the liability of drug manufacturers and insurance plans in the catastrophic phase. Current law requires drug manufacturers to pay 70 percent of costs in the coverage gap. In contrast, AAF’s proposal makes manufacturers liable for 9 percent of costs in the catastrophic phase; the Finance proposal puts their liability at 20 percent, likewise in the catastrophic phase; and Speaker Pelosi’s plan makes them liable for 10 percent in the initial coverage phase and then 30 percent in the catastrophic. Shifting manufacturer liability in this way ties the rebates more closely to the cost of the drug. The chart below is adapted from Table 3 in Hayes’ Insight and shows how much drug manufacturers would pay for a drug with a given price—in nominal terms and as a percentage of the drug’s price—under each plan compared to current law. While the underlying mechanisms for each plan vary, a consensus has emerged: Scrap the indirect rebate cap of $4,122 and replace it with an incremental rebate.
From Team Health
Daily Dish: Some Depressing Stats to Start Your Week – Douglas Holtz-Eakin, American Action Forum President
At a time of sweeping health care reform proposals, it seems like a no-brainer to focus some attention on a targeted problem like the maternal mortality rate.
Worth a Look
Axios: Small and large hospitals continue merger race
Reuters: Massachusetts set to defend vaping ban, toughest in nation, in court