Weekly Checkup
March 20, 2020
What Italy Can Teach Us About Reacting to the Coronavirus
As the public comes to grips with the critical actions necessary to curb the spread of COVID-19, we hear much about “flattening the curve” and “social distancing.” But why are these principles so important for protecting not just ourselves, but our broader society? Look to Lombardy, Italy.
As outlined in this Journal of the American Medical Association article, what began as a single case at the Codogno Hospital turned into a nightmare in one day. The first patient in Italy was a man in his 30s. Upon receiving a positive test, he was quickly admitted to the ICU so he could be treated in a more isolated setting. Unfortunately, within 24 hours, the number of cases went from one to 36, without the newly infected having any known contact with the first patient.
Within two weeks, ICUs saw a huge spike in COVID-19 admissions, complicated by the fact that ICUs in Lombardy were already at 85-90 percent occupancy. Despite rapidly expanding their ICU capacity, these hospitals soon started transporting ICU patients outside of the region to any ICU bed that would accept them. Linear and exponential growth models project between 869 and 14,542 ICU admissions in Italy by March 20th, with the extremes being far beyond their capacity to handle.
As of March 11th, doctors and nurses were already incapable of treating everybody, resorting to utilitarian “catastrophe medicine” measures. Such measures entail setting cutoffs for care based on age and comorbidities, distributing resources to where there is the highest probability of success, and sacrificing other patients in the meantime. Should the United States face a similar spike in the number of cases (understanding the substantial differences in the demographics and health care systems of these two countries), there is no reason to suspect the results would magically be different. By way of example, look at what is happening in Washington state, which has roughly a sixth of all U.S. cases and half of all deaths. On top of the growing number of cases, there is a shortage of basic personal protective equipment such as surgical masks, which are being used up at nearly three times the normal rate for this time of year, on top of other critical medical equipment shortages on the horizon.
While Italy has a much larger elderly population than the United States, the way this pandemic has hit them can provide a critical lesson on the importance of “overreacting” when things don’t appear that bad. It can be hard for people to grasp the nature of exponential growth, but such a visceral example in Italy helps demonstrate that under these growth conditions, a case or two turns into system collapse quite quickly should drastic measures not be taken at all levels, from individual behavior to national policy.
Emergency legislation like H.R. 6074 and bills such as H.R. 6201 serve a critical role in helping families as they self-isolate and slowing the resulting economic downturn. As AAF’s Isabel Soto and Tara O’Neill Hayes discuss here and here, however, there are considerations for H.R. 6201 that can optimize the targeting of funding to those who need it most while sparing some inefficiencies in monetary distribution for assistance programs such as paid sick leave.
On a positive note, at least it is now appropriate to wear sweats while you work from home.
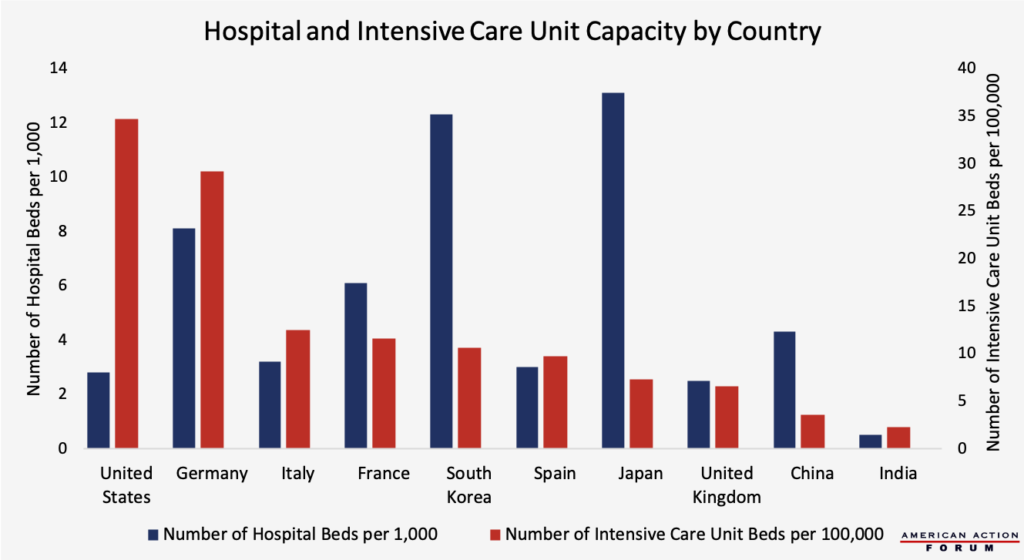
Chart Review: Hospital and Intensive Care Unit Capacity
Margaret Barnhorst, Health Care Policy Intern
The ongoing COVID-19 outbreak continues to raise questions about hospital infrastructure and capacity. As the chart below shows, although the United States has a lower overall hospital-bed capacity relative to other developed countries (2.8 beds per 1,000 inhabitants), the United States has a relatively high number of intensive care unit (ICU) beds (34.2 per 100,000 inhabitants). For comparison, Italy has only 12.5 ICU beds per 100,000 inhabitants and China only 3.6 ICU beds per 100,000 inhabitants. (These figures are all pre-pandemic, so they do not account for efforts to increase capacity.) The vast majority of COVID-19 cases are mild, but severe cases can result in respiratory failure that requires ventilation; around 10 percent of COVID-19-infected individuals in Italy required treatment in the ICU, and 5 percent of COVID-19-infected patients in China received critical-care treatment. Despite the advantage of having greater relative ICU capacity, the United States is still projected to have hospital-bed shortages by May if the problem continues at its current rate.
All data are from before the COVID-19 outbreak. Hospital capacity data source: OECD Health Statistics Database, ICU capacity compiled by Forbes (data sources: Intensive Care Medicine Journal, National Center for Biotechnology Information, and Critical Care Medicine Journal)
From Team Health
Daily Dish: Buy American – Coronavirus Edition – AAF President Douglas Holtz-Eakin
Using a pandemic crisis to foist costly medical protectionism on a panicked electorate is disappointing at best.
Daily Dish: H.R. 6201 – Douglas Holtz-Eakin
The House bill responding to the pandemic had some fairly straightforward enhancements to Medicaid, food programs, and unemployment insurance, along with two leave programs.
Estimating the Cost of the Families First Coronavirus Response Act – Isabel Soto, Labor Market Policy Data Analyst, and Tara O’Neill Hayes, Director of Human Welfare Policy
H.R. 6201 is expected to cost $183.8 billion, although if an important restriction on firm sizes were to be eliminated, the total cost could exceed $350 billion.
Daily Dish: Update on Coronavirus Response – Douglas Holtz-Eakin
Last Friday saw important developments in the response to the coronavirus pandemic at both ends of Pennsylvania Avenue, along with some purely political pandering.
Worth a Look
New York Times: A Promising Treatment for Coronavirus Fails
Wall Street Journal: Why Dr. Anthony Fauci Runs