Insight
April 21, 2023
FY2024 Inpatient Prospective Payment System and Long-Term Care Hospital Prospective Payment System Proposed Rule
Executive Summary:
- The Centers for Medicare and Medicaid Services’ (CMS) 2024 Inpatient Prospective Payment System (IPPS) and Long-Term Care Hospital Prospective Payment System (LTCH PPS) proposed rule includes a 2.8 percent increase for the IPPS payment rate; this would result in an increase of $2.7 billion in total payments for inpatient hospitals, while the LTCH PPS payment rate would increase by 2.9 percent to a total of over $2.6 billion.
- Under the proposed rule, Disproportionate Share Hospitals would see a drop of 2.4 percent in uncompensated care and supplemental payments for an expected aggregate amount of over $6.7 billion, a decrease of $161 million from 2023 due in part to the end of COVID-19 supplemental payments and an expected drop in Medicaid enrollment.
- CMS also proposed updates to rural and low-wage hospital wage index calculations, changes to quality reporting and value-based purchasing measures, and increased restrictions on physician-owned hospitals.
Introduction
On April 10, 2023, the Centers for Medicare and Medicaid Services (CMS) released its fiscal year (FY) 2024 Inpatient Prospective Payment System and Long-Term Care Hospital Prospective Payment System (IPPS/LTCH PPS) proposed rule. This proposed rule sets payment rates for acute care inpatient and long-term care hospitals, and makes adjustments to IPPS and LTCH policies for FY2024, among other modifications. This paper explains the rule’s notable changes to the IPPS and LTCH PPS, including expected changes to payment rates, safety-net hospital policy, rural hospital payments and policy, quality reporting and value-based purchasing rules, and physician-owned hospitals.
The Proposed Rule
Payment Rates
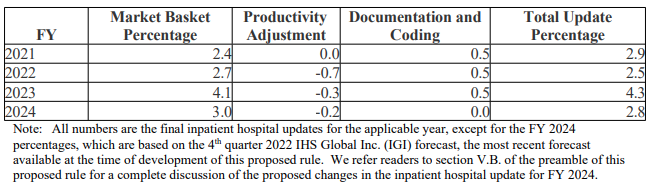
The IPPS payment rate will receive a 2.8 percent increase for hospitals that submit quality reporting data and are considered meaningful electronic health record (EHR) users. This increase is derived from the 3 percent cost increase in CMS’ market basket, which measures the change in price for a select mix of goods and services over time. A productivity adjuster of 0.2 percentage points is then applied, yielding the 2.8 percent increase. Hospitals that submit quality data but are not meaningful EHR users will receive only a 0.55 percent increase in payments, and those that do not submit quality data but are meaningful EHR users will see a 2.05 percent increase. Hospitals that neither submit quality data nor are considered meaningful EHR users will receive a 0.2 percent decrease in payments. CMS expects these changes to result in a $3.2 billion increase in operating and capital payments to acute care hospitals, and after factoring in a $460 million decrease in new technology add-on payments (NTAPs) due to expiring NTAPs for several technologies, CMS predicts acute care hospitals will see a total increase in payments of $2.7 billion in FY2024. Figure 1 shows changes in payment update percentages since FY2021.
Figure 1.
Source: CMS FY2024 Proposed Rule
The LTCH PPPS will see the standard payment-rate increase of 2.9 percent, while LTCHs that fail to submit quality reporting data will see an increase of only 0.9 percent. Due to a 4.7 percent decrease in high-cost outlier payments, CMS expects total LTCH PPS payments for standard payment rate cases (as opposed to site-neutral payment rate cases) will decrease by 2.5 percent, or around $59 million, in FY2024. Some of this aggregate decrease will be canceled out by the general standard rate increase. In total, CMS estimates that FY2024 LTCH PPS payments will amount to a total of just over $2.6 billion, a decrease of around $24 million from FY2023.
Safety-Net Hospitals
Disproportionate Share Hospitals (DSHs) will see a drop of 2.4 percent in uncompensated care and supplemental payments, totaling slightly over $6.7 billion in uncompensated care and supplemental payments for FY2024, compared to just under $6.9 billion for FY2023 – a decrease of roughly $161 million, not including $90.3 million set aside for Indian Health Services (IHS), Tribal, and Puerto Rican hospitals. Urban DSHs are expected to see an average DSH payment decrease of 2.69 percent, while rural DSHs are expected to see an average decrease of 2 percent. This decrease is the result of several changes to different payment calculation factors, including the ceasing of COVID-19 supplemental payments and the expected decrease in Medicaid enrollment as the public health emergency ends. See Figure 2 for historical uncompensated care and supplemental payments since FY2021, excluding IHS, Tribal, and Puerto Rican hospitals.
Figure 2.
| FY | Total Uncompensated Care & Supplemental Payments (in billions of dollars) | Percent Change |
| 2021 | $8.290 | -0.7 |
| 2022 | $7.192 | -13.2 |
| 2023 | $6.874 | -4.4 |
| 2024* | $6.713 | -2.4 |
| *Proposed |
CMS is seeking comment on the challenges safety-net hospitals face, and in particular how CMS should measure the degree to which a hospital functions as a safety-net facility. CMS is also seeking feedback on the usefulness of the Medicare Payment Advisory Commission’s “Safety-Net Index,” along with other potential measures of a hospital’s safety-net status.
Rural Hospitals
For geographically urban hospitals that have reclassified as rural for payment purposes, CMS proposes including these hospitals’ wage data in its calculation of the wage index for a rural area of the state. Statutorily, the wage index for any hospital in an urban area of a state cannot be lower than the wage index for any hospital in a rural area (known as the rural floor). While reclassified hospitals may not necessarily be subject to the rural hospital wage index, they are required by law to be treated as geographically rural. Thus, CMS holds that their data must be included in its calculation of a state’s rural wage index. , See this American Action Forum primer for more information about geographic adjustment on hospital wage indexes.
CMS proposes to continue for another four years its temporary low-wage hospital policy begun in FY2020, whereby CMS provides an increased wage index for hospitals falling below the 25th percentile of the Medicare inpatient hospital wage index (which includes many rural hospitals). This rule allows these low-wage hospitals to increase compensation for employees without the corresponding multi-year lag in Medicare recognition of and reimbursement for the increase.
Additionally, CMS proposes to allow rural hospitals that become Rural Emergency Hospitals (REH) to serve as training sites for Medicare graduate medical education purposes. REHs are hospitals that must functionally eliminate inpatient beds but will receive additional payment support in return.
Quality Reporting and Value-Based Purchasing
CMS proposes nine different actions with regard to the Hospital Inpatient Quality Reporting (IQR) Program, three of which affect the Hospital Value-Based Purchasing (VBP) Program. First, CMS proposes adding three new electronic clinical quality measures (eCQMs) from which hospitals can choose to meet eCQM reporting requirements for a given year. Second, CMS proposes modifying three current quality reporting measures to include Medicare Advantage admissions in two of these measures. It would also update the third regarding COVID-19 vaccinations to track how many health care personnel are up to date with COVID-19 vaccinations. Finally, CMS proposes removing three measures from the Hospital IQR Program, adding two of these to the VBP Program, and eliminating the third regarding elective delivery of babies prior to 39 weeks. The elective delivery measure being eliminated is considered “topped-out” by CMS, meaning performance is so high that distinctions between hospitals are no longer meaningful.
The LTCH Quality Reporting Program (QPR) is also being adjusted, with CMS proposing to include in reporting the percentage of patients and health care workers at LTCHs with up-to-date COVID-19 vaccinations. Additionally, CMS proposes to adopt a Functional Discharge Score (DC Function) measure, which would assess the percentage of LTCH patients who meet or exceed an expected discharge function score. The DC Function measure would replace a current measure that is considered topped-out. Finally, CMS proposes requiring LTCHs to report 100 percent of required quality measure and patient assessment data on 90 percent of assessments submitted to CMS, up from the current 80 percent of assessments needing 100 percent of quality measure and patient assessment data.
Physician-Owned Hospitals
While the Affordable Care Act outlawed the creation of new physician-owned hospitals (POHs), existing POHs at the time of the law’s passage were allowed to continue, albeit with a functional ban on expansions to their facilities. POHs are allowed to request exceptions to the ban on expansion. CMS proposes to add further barriers to existing POH expansion, including reinstating restrictions on both the frequency of expansion exception requests for “high Medicaid facilities” as well as the location of expansion facility capacity.