Research
November 24, 2020
Background: The Relationship Between External Factors and Chronic Disease
Executive Summary
- In addition to various socioeconomic factors and a person’s lifestyle, there are numerous external, community-level factors that affect a person’s propensity to develop a chronic disease, such as the environment, access to nutritious foods, access to quality health care, and the safety and social supports of the surrounding community.
- Similar to more personal socioeconomic factors affecting one’s health, many of these factors are highly correlated with one another, and in particular, with one’s income.
- Given the high prevalence and high cost associated with chronic disease, it is important to understand the connections between these risk factors so that any policy solutions can be appropriately targeted.
Introduction
There is an abundance of factors that impact an individual’s likelihood of developing a chronic disease. Previous American Action Forum research explored the relationship between chronic disease and individual-level determinants such as education, income, and family history. This paper examines the health impact of risk factors that exist beyond the individual level—although these external factors are often related to individual-level ones. Exposure to pollutants, access to health care and nutritious food, and community dynamics all contribute to an individual’s risk of developing a chronic disease. Income is a predominant driver of these elements; adults living at the federal poverty level are over five times more likely to report health issues than those with incomes at least four times the federal poverty level.[1]
For information regarding policy interventions that could address these risk factors, click here.
External Risk Factors Relating to Chronic Disease
Access to Nutritious Food
Health experts agree that nutrition plays a vital role in an individual’s health and the likelihood of developing a chronic disease.[2] Diets directly affect the risk of obesity, a chronic disease that can exacerbate or increase the likelihood of other chronic diseases. Nutrition also affects the ability to learn and focus in school, and success in school also influences the risk of chronic disease. Consumption of fresh produce is an essential aspect of receiving adequate nutrition.[3] Specific nutrients have been linked with chronic disease prevention. For example, potassium, calcium, and magnesium, all found in abundance in fresh fruits and vegetables, have been found to play significant roles in staving off cardiovascular disease.[4] The relatively high price of fresh foods versus processed foods and the prevalence of food deserts in the United States reduce access for many Americans.
Affordability
Income is linked to the consumption of nutritious foods both directly and indirectly. Low-income groups are more likely to purchase cereals, pasta, potatoes, legumes, fatty meats, and canned or frozen fruits and vegetables.[5] This choice is driven by these foods’ price relative to fresher foods, longevity, convenience, and energy-density.[6] When income is severely restricted, many low-income families make the choice to forgo certain meals altogether. Children growing up in these environments develop poor eating habits that can severely impact their health. These children are more likely to skip breakfast, indulge in fast food, and eat few family-prepared meals.[7] They also feel more hopeless about their dietary situation and tend to opt for foods that contain empty calories such as sweets and fried foods.[8]
Government programs and regulations also impact the price and affordability of food. The Supplemental Nutrition Assistance Program (SNAP) and the Women, Infants, and Children (WIC) program provide financial subsidies for the purchase of certain food items, though there are restrictions on who is eligible and which foods may be purchased. The School Breakfast Program and School Lunch Program help ensure children have access to food meeting certain nutritional requirements while at school by providing free or reduced-cost meals to students, based on family income.[9]
Distance
Food deserts are generally defined as geographic areas where the inhabitants do not have sufficient access to affordable, healthy food due to the absence or limited number of stores that have it within a reasonable traveling distance.[10] The relationship between income and race is often a driver of this phenomenon. One study found that wealthy neighborhoods had three times the number of grocery stores than poor neighborhoods, and majority White neighborhoods had four times the number of grocery stores than majority Black neighborhoods.[11] The distance people need to travel to obtain healthy food directly impacts consumption. The same study found that for every additional supermarket within the neighborhood, produce consumption increased by 32 percent.[12] It is also important to note the relationship between the incidence of healthy food providers and income. Consumption could be increasing as a result of enhanced proximity, but people living near grocery stores are also more likely to have the income necessary to afford to purchase fresh produce.
Access to Quality Health Care
Access to quality health care can affect an individual’s awareness and control of an existing chronic disease or chronic disease risk.[13] Access can be characterized by the degree to which someone can afford quality health care and the geographical distance between the home and quality health services.
Affordability
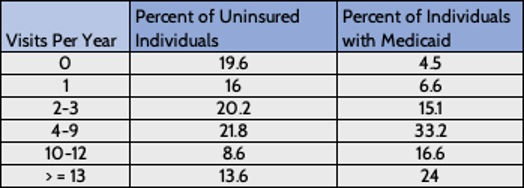
Insurance is a key component of affordability. A lack of insurance is associated with lower rates of preventative care, delays in care, forgone care, medical bankruptcy, and increased mortality.[14] Those with incomes too low to afford private insurance or who hold jobs where insurance isn’t provided may have the option of applying for Medicaid. Many low-income individuals still remain uninsured, however, particularly in states that have not expanded their Medicaid eligibility thresholds.[15] Copayments, a lack of awareness about eligibility, and application complexity can be barriers to enrollment.[16] Medicaid coverage facilitates outpatient care, which is associated with improved control of blood pressure, awareness of being overweight, lowered depression rates, and increased diagnoses of diabetes.[17] Among those with a chronic disease, outpatient service utilization diverges at higher rates of usage between Medicaid recipients and the uninsured. The table below shows how an individual’s lack of insurance tends to reduce their use of health care. Ironically, limiting care in the short-term can lead to such poor health that many visits are needed later.
Source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4695932/
Distance
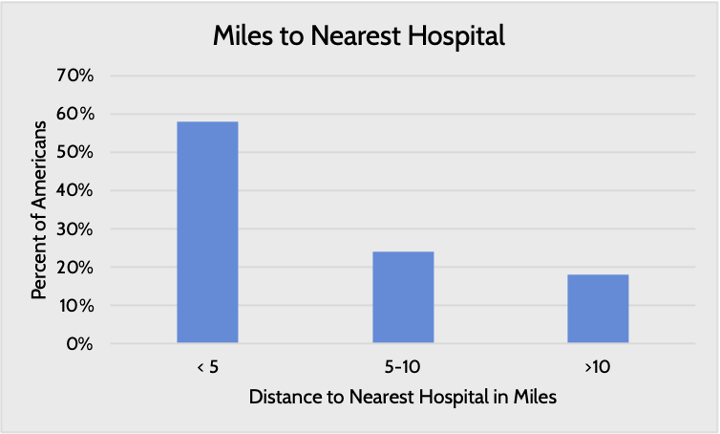
The distance to the nearest health provider varies by the region and income level of the residential areas. Nearly 20 percent of Americans live more than 10 miles away from their nearest hospital. Large swaths of the country are designated as health professional shortage areas, whether for primary care, dental care, or mental health care.[18]
Source: Pew
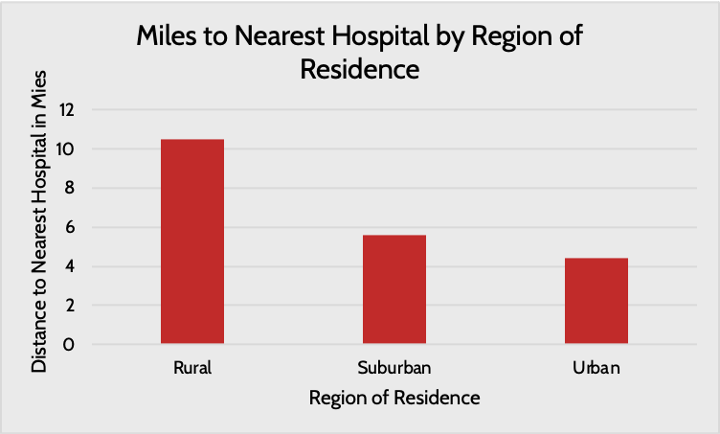
Further, the types of hospitals people have access to vary: People living in rural areas typically do not have access to academic research hospitals providing cutting-edge care, and the limited resources available in rural settings often make it difficult to provide high-quality care.[19] A lack of access to specialists in rural areas is a key challenge.[20]
Income level is similarly correlated with the geographical availability of health care. Poor areas, where residents are often less healthy than in wealthier areas, are more likely to face physician shortages and closed hospitals.[21] In fact, approximately 58 percent of the 5,800 “primary care shortage” areas identified by the federal government are located in high-poverty census tracts.[22] This phenomenon is caused by a multitude of factors, including an understandable unwillingness or inability for physicians and hospitals to operate in areas where patients are less likely to be able to pay their bills, as well as a lack of interest among many providers to live in rural or poorer areas. As a result, individuals living in these areas either do not seek medical help or do so in inefficient ways. For example, a 2012 National Health Survey found that 80 percent of people who used the emergency department that year cited a lack of access to other forms of care as the reason for their visit.[23]
Pollution
Pollution of natural resources such as water and air has devastating impacts on health.[24] Pollutants enter the environment in a variety of ways and have a multitude of sources. Toxic metals from manufacturing processes, chemicals from agriculture, and fragrances from cosmetic products are all examples of physically harmful pollutants.[25] Scientists have drawn links between such substances and neurocognitive impairment, vascular disease, obesity, and, most often, cancer.[26] In fact, a substantial proportion of all cancer is caused by environmental and occupational exposures to toxins.[27] Additionally, exposure to just the mean amount of air pollution has been shown to increase the risk of Parkinson’s, Alzheimer’s, and related dementias.[28]
Some low-income individuals are more at risk of these kinds of exposures due to the environments in which they live and the nature of their employment. For example, in California, households earning less than $20,000 a year and people who don’t own cars face vehicle pollution levels 20 percent higher than the state average.[29] High manual labor jobs that offer lower wages are breeding grounds for toxins. People working these jobs can inhale hazardous particles or come in direct contact with toxic substances. Miners and those who do stonework or sandblasting run the risk of exposure to crystalline silica, which increases the risk of silicosis-related mortality.[30] Additionally, substances such as asbestos, commonly found in these work environments, can cause lung cancer.[31]
To be sure, as shown by the chart below, not all low-income individuals are equally at risk of exposure to pollutants. Some high-poverty areas have relatively high numbers of good quality air days, particularly more rural areas where there is less industry. Other rural areas, however, have relatively poor air quality, which results from agricultural activity, wildfires, and downwind effects from more industrialized areas.[32]
Sources: U.S. Census Bureau, EPA
Public Safety and Community Dynamics
Safety impacts health in direct and indirect ways. Being exposed to violence brings potential life-long health issues, but fearing that you may be the victim of violence can also create behavioral changes that impact your health. The impact of exposure to violence at a young age can be particularly damaging. Children can experience long-term behavioral problems, depression, anxiety, and post-traumatic stress disorder.[33] These mental health issues can lead to a greater risk of substance abuse, risky sexual behavior, unsafe driving, and domestic violence in adulthood.[34] Fear of becoming a victim of violence can also impact community members’ health by influencing their level of participation in both physical and social activities. Residents who don’t feel safe in their communities are less likely to form meaningful relationships with other community members, increasing the risk of isolation.[35] Social isolation has been shown to increase the risk of almost every chronic disease. Isolation increases a person’s risk of premature death and inflates a person’s risk of developing dementia by 50 percent, heart disease by 29 percent, and stroke by 32 percent. Additionally, social isolation contributes to the development of mental health issues such as depression and anxiety, and can increase the incidence of suicide.[36] People who perceive their communities as unsafe also engage in less physical activity.[37] A lack of physical activity increases the risk of obesity, diabetes, and high blood pressure.[38] All of these effects are more likely to be felt by low-income communities as crime rates are higher in these areas.[39]
Community dynamics refers to the social cohesion and culture of a community. Many behaviors related to health—healthy eating, substance use, physical exercise—are influenced by one’s peers. Studies show that members of tight-knit communities are more likely to take care of one another by, for example, encouraging physical activity, providing information regarding support services, and reducing the isolation that can lead to depression, all of which contributes to improved health.[40]
Transportation
Modes of transportation can affect how easily and, ultimately, how frequently an individual can seek health care, as well as access other things that impact an individual’s health such as good nutrition, a job, and education. Lack of access to reliable, affordable transportation can lead to missed appointments, delayed care, and missed or delayed medication use.[41] Missed or delayed care can exacerbate pre-existing chronic conditions, prevent the proper diagnosis and treatment of new diseases, or indirectly contribute to the development of new diseases by allowing others to go untreated. Ownership or reliable access to a car has been shown to be positively correlated with greater utilization of health care.[42] On the other hand, people who rely on public transit or walking are more likely to not have a regular source of care and are more likely to delay care.[43] These effects can be especially pronounced in rural areas where public transportation may not even be an option. Conversely, cars in urban areas may be unrealistic due to expense and parking limitations; further, people may be unable to drive as a result of prior offenses.[44]
People also need reliable transportation to get to school or work, as being stranded is likely to hinder people’s ability to succeed in either, while both are important contributors to one’s health. A lack of reliable transportation also makes it more difficult to acquire groceries, and while reliable public transportation is better than nothing, it is difficult to haul more than a few days’ worth of groceries on the bus or subway, making access to a car more valuable.
Conclusion
Community-level risk factors are often rooted in individual-level risk factors: education, income, race, mental health, lifestyle, and family history. This analysis further explores the intersections among chronic disease risk factors. This correlation is a key reason why the difference in chronic disease prevalence between high-income and low-income individuals is so stark. The many underlying factors associated with low incomes—limited access to health care, lower rates of education, poor nutrition, and other systemic issues—help drive this phenomenon.
[1] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5171223/
[2] https://www.sciencedirect.com/science/article/pii/S0271531718302227
[3] https://www.choosemyplate.gov/eathealthy/vegetables/vegetables-nutrients-health
[4] https://link-springer-com.proxy.library.cmu.edu/book/
[5] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2847733/
[6] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2847733/
[7] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3794652/
[8] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3794652/
[9] https://www.fns.usda.gov/sbp/fact-sheet, https://www.ers.usda.gov/topics/food-nutrition-assistance/child-nutrition-programs/national-school-lunch-program/
[10] https://foodispower.org/access-health/food-deserts/
[11] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3794652/
[12] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3794652/
[13] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4695932/
[14] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4695932/
[15] https://www.cbpp.org/research/health/states-that-have-expanded-medicaid-are-better-positioned-to-address-covid-19-and
[16] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3794652/#:~:text=more%20chronic%20diseases.-,Racial%2Fethnic%20minorities%20are%201.5%20to%202.0%20times%20more%20likely,seem%20to%20be%20getting%20worse.
[17] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4695932/
[18] https://data.hrsa.gov/maps/map-gallery
[19] https://www.ruralhealthinfo.org/topics/health-care-quality, https://rhrc.umn.edu/publication/rural-urban-differences-in-medicare-quality-scores-persist-after-adjusting-for-sociodemographic-and-environmental-characteristics/
[20] https://www.sciencedaily.com/releases/2019/12/191203160602.htm
[21] https://newsinteractive.post-gazette.com/longform/stories/poorhealth/1/
[22] https://newsinteractive.post-gazette.com/longform/stories/poorhealth/1/
[23] https://www.cdc.gov/nchs/data/nhis/earlyrelease/emergency_room_use_january-june_2011.pdf
[24] https://www.who.int/airpollution/ambient/health-impacts/en/, https://www.hindawi.com/journals/jeph/2012/356798/
[25] https://www.hindawi.com/journals/jeph/2012/356798/
[26] https://www.hindawi.com/journals/jeph/2012/356798/
[27] https://www.env-health.org/IMG/pdf/110913_HEAL_fact_sheet_-_Chronic_disease_and_environment-final.pdf
[28] https://www.thelancet.com/journals/lanplh/article/PIIS2542-5196(20)30227-8/fulltext
[29] https://www.calhealthreport.org/2019/02/08/people-of-color-and-the-poor-disproportionately-exposed-to-air-pollution-study-finds/
[30] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3813007/
[31] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3813007/
[32] https://www.earth.columbia.edu/articles/view/3281, https://www.epa.gov/air-research/wildland-fire-research-health-effects-research, https://www.epa.gov/interstate-air-pollution-transport/what-interstate-air-pollution-transport
[33] https://www.healthypeople.gov/2020/topics-objectives/topic/social-determinants-health/interventions-resources/crime-and-violence
[34] https://www.healthypeople.gov/2020/topics-objectives/topic/social-determinants-health/interventions-resources/crime-and-violence
[35] https://www.ca-ilg.org/health-public-safety
[36] https://www.cdc.gov/aging/publications/features/lonely-older-adults.html
[37] https://www.healthypeople.gov/2020/topics-objectives/topic/social-determinants-health/interventions-resources/crime-and-violence
[38] https://www.ca-ilg.org/health-public-safety
[39] https://www.healthypeople.gov/2020/topics-objectives/topic/social-determinants-health/interventions-resources/crime-and-violence
[40] https://www.lisc.org/media/filer_public/3c/12/3c122f2a-41e1-4233-9d68-e5989be210b6/healthassessmentreport_final_shrunk.pdf, https://scopeblog.stanford.edu/2011/06/16/community-dynamics-play-an-essential-role-in-fighting-obesity/
[41] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4265215/
[42] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4265215/
[43] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4265215/
[44] https://www.americanactionforum.org/insight/the-implications-of-relying-on-monetary-penalties-in-the-u-s-criminal-justice-system/