Research
March 9, 2022
The Economic Costs of Poor Nutrition
Executive Summary
- Poor nutrition is a key risk factor for numerous chronic diseases, most notably obesity, heart disease, type 2 diabetes, and as many as 13 types of cancer.
- These diseases reduce a person’s likelihood of working, and those who do work are less likely to work full-time and as productively as their peers without chronic disease.
- The economic implications of nutrition-related chronic disease are primarily reduced wages, higher employment costs, and reduced government revenue.
- This analysis estimates the economic cost of the four nutrition-related chronic diseases among 18 to 64-year-olds at $16 trillion from 2011-2020 (or nearly 9 percent of gross domestic product annually) after accounting for direct health care costs, lost productivity, and lost wages.
Introduction
Poor nutrition is more than a health care concern; it also has tremendous, multifaceted economic implications. Poor diet leads to numerous chronic diseases, often resulting in disability and premature death. This deprives individuals of their health and quality of life, as well as their productive potential, hindering their efforts to work full-time or at all, leading to lower wages. For employers, absenteeism, functional limitations among their employees, and the provision of health insurance pose tremendous costs. Nationally, the quality and quantity of the labor force determines economic output and government revenues. Simultaneously, demands for government resources increase as people incur greater health care costs and become more dependent on assistance when they are unable to work. Consequently, poor nutrition is a large and rapidly growing burden for the United States.
This analysis estimates the health and economic costs of the four most common nutrition-related chronic diseases—heart disease, obesity, type 2 diabetes, and as many as 13 types of cancer —among the working-age population. To do so, we estimate the health care costs directly associated with these diseases, the indirect costs due to lost productivity and lower wages, and lost government revenue resulting from those lower wages and reduced employment. This analysis estimates the total economic cost from 2011-2020 at $16 trillion, or nearly 9 percent of gross domestic product (GDP) annually.[i] Of note, this estimate does not account for premature death or reduced lifetime earnings, which other estimates suggest would significantly increase this cost.[ii] Further, it does not account for comorbidities often associated with these diseases, such as depression and chronic pain, which are also known to significantly decrease productivity.[iii]
Scope of the Problem
Poor nutrition is associated with the most common chronic diseases in the United States: obesity, heart disease, stroke, type 2 diabetes, and as many as 13 types of cancer (which account for 40 percent of all cancers diagnosed in the United States).[iv] Obesity now affects 42 percent of American adults, or 109.5 million individuals.[v] Even more Americans are estimated to have cardiovascular disease: 49.2 percent, or 126.9 million people in 2018; although, when excluding hypertension, this rate falls to 9.3 percent, or 26.1 million in 2018.[vi] More than 33 million Americans have type 2 diabetes.[vii] In 2018, there were an estimated 6.5 million people living with nutrition-related cancer.[viii]
Given that obesity is highly associated with each of these other diseases, there is significant overlap in the people who are affected by these diseases and thus simply adding up the prevalence for each would overestimate the number of people afflicted by nutrition-related disease.[ix] That said, it is estimated that at least 117 million American adults were living with nutrition-related chronic diseases as of 2017, many of whom will die prematurely as a result. In 2016, poor diet was the greatest risk factor for death in the United States and the third leading cause of morbidity, accounting for more than 500,000 deaths and 11 percent of all disability-adjusted life years lost (the number of years either lost or not lived in full health due to disability).[x] With the prevalence of obesity increasing at roughly 2 percent per year, this burden is expected to worsen for the foreseeable future.
Calculating the Costs
In estimating the health and economic costs associated with poor nutrition, this analysis considers the prevalence of the four primary nutrition-related chronic diseases among the working-age population (18 to 64 year-olds), the health care costs associated with each disease, the effect of each disease on a person’s likelihood of missing work or ability to be productive at work, the likelihood of being unemployed because of chronic illness, and the consequential impact on government revenues as a result of lower wages and the growing need for assistance.
Details regarding data sources and specific cost and prevalence considerations can be found in the Methodology appendix. Most prevalence figures come from government health agencies, while cost and productivity figures are sourced from available literature on the subject. Projections for economic costs are largely based on data from the Bureau for Labor Statistics.
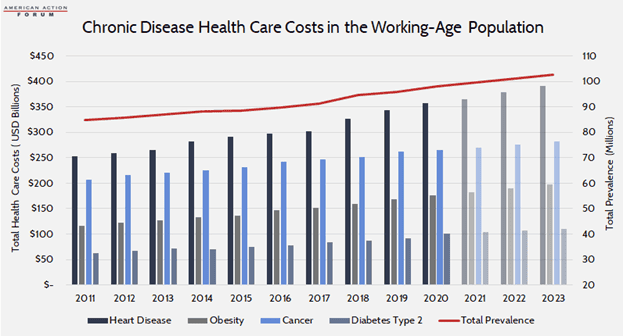
Direct Health Care Costs
The incremental health care costs associated with each disease range from an estimated $2,500 for obesity (in 2017) to nearly $80,000, on average, for treating any of the 13 identified types of cancer. From a societal perspective, however, heart disease—at a cost of more than $20,000 per person—is the most expensive overall due to its prevalence. Although, when considering obesity as a risk factor for these (and other) diseases, it is estimated to be responsible for 44 percent of all direct health care costs in the United States.[xi] In total, between 2011-2020, these four diseases cost an estimated $7.6 trillion. Over the following three years (2021-2023), these diseases will cost an estimated $2.9 trillion.
These costs are borne by individuals, their employers, and the government, with variations largely dependent on whether or how individuals are insured. For those with employer-sponsored insurance, employers typically pay 70-80 percent of health care premiums, which are intended to cover the bulk of an average individual’s annual health care costs.[xii] Of course, individuals with any of these chronic conditions likely have higher-than-average costs and will likely face significant out-of-pocket costs. That said, many of these individuals are likely low-income, as having a low income is a strong risk factor for chronic disease.[xiii] As such, many who have nutrition-related chronic disease are likely covered by Medicaid, in which case most costs are covered by the government (state and federal). Two-thirds of Medicaid beneficiaries are overweight or obese, 28 percent have hypertension, and 26 percent report being in poor health.[xiv] The remainder are likely uninsured, in which case the individual would bear the brunt of the costs.
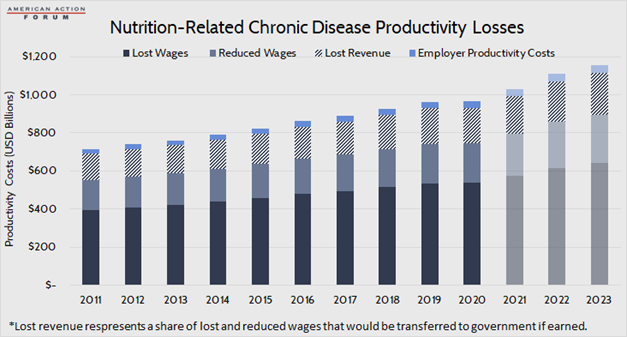
Indirect Costs: Lost Wages, Lower Productivity, and Reduced Revenues
The indirect costs associated with chronic disease similarly fall across the same parties. While there are manifold indirect costs, some of which are difficult to quantify, this analysis focuses on lower wages, productivity costs to employers, and foregone government revenues.
Individuals
The financial burden of chronic illness is felt most acutely at the individual level. The primary indirect cost is lost wages—whether from an inability to work at all or as much as one otherwise would if they were healthy. Household income and savings are invariably diminished, continuing the downward spiral of poor health and poverty. Studies estimate that chronic disease reduces one’s wages anywhere from 6 percent to as much 18 percent.[xv] This is felt distinctively by men and women in the workforce; women with chronic disease face a larger percentage reduction in wages, and men face a greater reduction in the number of hours worked.[xvi] This effect compounds over time: chronic illness will cost the individual progressively more as health care costs increase and the effect of missed promotions and raises flattens one’s lifetime earning potential. Individuals also lose out on the benefit of compounding interest when they are unable to save which may severely limit one’s financial stability in retirement.[xvii] Further, just as poor health can reduce employment and thus income, poor economic conditions can cause poor health. Unemployment is associated with reduced consumption of fruits and vegetables and increased consumption of snacks and fast food which may exacerbate existing health problems.[xviii]
Chronic disease also keeps many people out of the labor force altogether. One study found that chronic disease reduces employment by 5 percentage points, which translates to nearly 12 million fewer people working each year over the past decade.[xix]
Between the reduction in wages among those unable to work as much or to be as productive as they otherwise would and the foregone wages from an inability to work at all, it is estimated that that the overall reduction in wages due to obesity, heart disease, type 2 diabetes, and nutrition-related cancer totaled $8.1 trillion between 2011-2020. Reduced wages among the working accounts for 28 percent of lost income. It is estimated that another $3.2 trillion in wages will be lost from 2021-2023.
Employers
Employers face costs due to reduced output when workers miss time at work (absenteeism) or are less productive at work because of limitations from their disease (presenteeism); although, these costs—particularly related to presenteeism—are often passed through to workers in the form of reduced wages, as discussed.[xx] In 2019, U.S. employers lost an estimated half a trillion dollars in productivity costs, resulting from 978 million days lost due to illness and another 540 million lost workdays due to underperformance on the job; note, however, that this estimate is for all chronic disease, not just those being considered here.[xxi] This analysis of the cost to employers is based on a study from 2008 that estimated the amount of time over the course of a year that individuals’ ability to work was adversely impacted due to various chronic diseases. Many studies have been done on this subject—some finding higher costs, some lower—but this analysis used this particular study because it included per-person costs for each of the four diseases considered here. Those costs are adjusted each year by changes in the average cost of compensation, just as was used in the original estimate.
Among obesity, heart disease, diabetes, and cancer, cancer tends to have the largest impact on an employee’s productivity as treatment can be a long and debilitating process. It was estimated that in 2008, employees with cancer cost their employers an average of $1,601 in lost productivity over the course of the year compared with $200-$300 for obesity, heart disease, or diabetes.[xxii] These estimates are based on an average of 54.9 hours of reduced productivity per year, per person with cancer, 11.2 hours per person with heart disease, 11.1 hours per person with diabetes, and 7 hours per person with obesity. Based on average annual prevalence over the past decade, and assuming an 8-hour workday, this totals 113.5 million days of lost productivity as a result of these four diseases, annually. After considering average annual compensation costs, this productivity loss cost employers $295.9 billion from 2011-2020. It is estimated employers will lose another $114.4 billion from 2021-2023.
Government
In addition to individuals and employers, federal and state budgets also suffer from nutrition-related chronic disease as the resulting lower wages and employment reduces government revenues. Using a simple average tax rate of 20 percent, this analysis estimates that between 2011-2020, government revenues were reduced by $1.6 trillion as a result of these four chronic diseases. Between 2021-2023, another $636 billion will likely be forgone. Note that these lost revenues are a share of—not in addition to—individuals’ lost wages.
Simultaneously, more people will require government assistance because of their lower incomes. So, while less money is coming in, more money must be spent, squeezing the budget from both ends.
Those who are unable to work because of diet-related illness may qualify for several federal assistance programs, either directly because of a disability or because of the resulting loss of income, including Medicaid, Social Security Disability Insurance (SSDI), and the Supplemental Nutrition Assistance Program (SNAP).
An estimated 3 percent of SSDI recipients have endocrine, nutritional, or metabolic diseases.[xxiii] Based on an average monthly payment of nearly $1,400 as of December 2021 and 280,000 recipients, these individuals receive assistance of roughly $4.6 billion annually.[xxiv]
There is strong evidence that SNAP is associated with obesity, although it is unclear to what degree SNAP contributes to obesity or whether people who are already obese are more likely to become SNAP recipients.[xxv] People who are disabled may be eligible for SNAP.[xxvi] Assuming 3 percent of disabled SNAP beneficiaries are disabled due to nutrition-related disease (the same as with SSDI) and an average monthly benefit of $216 per person, nutrition-related disability is responsible for an estimated cost of $280.8 million per year, as of 2021.[xxvii]
There are likely many others who are eligible for SNAP, Medicaid, and other income-related assistance programs because of nutrition-related earnings challenges as previously mentioned, though it is difficult to quantify how many.
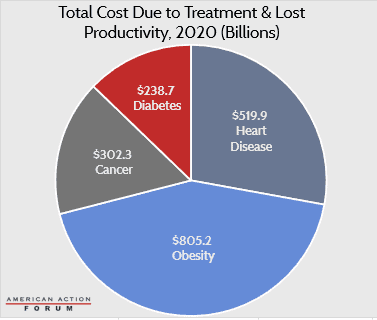
Total Costs
In total, after considering increased health care costs, lost wages, lost productivity, and lost revenue (which is a share of lost wages), this analysis estimates that obesity, heart disease, type 2 diabetes, and the 13 nutrition-related cancers identified cost the U.S. economy $16 trillion between 2011-2020. From 2021-2023, as prevalence continues to grow and costs escalate, it is estimated that the U.S. economy will lose another $6.1 trillion because of these diseases.
There are also other, sometimes less tangible costs incurred as a result of these diseases that are not accounted for in this analysis. For example, the stress and lost earnings incurred by family members who may have to spend time caring for a sick loved one. Poor nutrition early in life can cause underdevelopment of the brain resulting in mental and behavioral delays that could hinder one’s economic success later in life.[xxviii]
Conclusion
Poor nutrition has vast physical and economic consequences. Most Americans have a poor diet, leading to a high prevalence of various chronic diseases. These diseases may cause minor disruptions or hindrances to normal life for some while being severely debilitating for others. Overall, nutrition-related chronic diseases cause reductions in productivity, lost wages, and reduced economic output. This translates to reduced revenue for the federal government while simultaneously requiring more spending to treat the disease and provide economic assistance for those unable to work to their full potential because of illness. This analysis estimates that the overall economic cost of obesity, heart disease, type 2 diabetes, and nutrition-related cancers totaled $16 trillion between 2011-2020.
Appendix: Methodology
This analysis focuses on four common chronic diseases most closely associated with poor nutrition: obesity, heart disease, type 2 diabetes, and 13 types of cancer. Prevalence estimates are for those aged 18-64 to more closely reflect the working-age population. Prevalence and per-person health care cost estimates were sourced separately for each disease after a thorough review of recent studies:
Heart Disease
- Prevalence: CDC, National Center for Health Statistics
- Cost: “Medical Care Costs Among Patients With Established Cardiovascular Disease” (used average cost for patients without diabetes so as to assist with not double counting those costs and subtracted the approximate cost of someone with no chronic conditions (roughly $2,000))
Obesity
- Prevalence: Behavioral Risk Factor Surveillance System
- Cost: “Direct medical costs of obesity in the United States and the most populous states”
Cancer (13 Types)
- Prevalence: NIH SEER Explorer (2018); Annual Incidence: CDC Wonder
- Cost: NIH: Financial Burden of Cancer Care (average for each of the 13 nutrition-related cancers; includes initial and continuing care costs)
Diabetes, Type 2
- Prevalence: CDC Diabetes Atlas (Total diabetes prevalence among 18 to 64 year-olds increased by 20 percent to account for undiagnosed, then reduced by 10 percent to isolate type 2)
- Cost: American Diabetes Association, “Economic Costs of Diabetes in the U.S. in 2017” (costs attributed to diabetes for individuals under 65)
After obtaining health care cost estimates for a given disease in a given year, that base year estimate was increased or decreased by the annual percentage change in CPI-medical obtained from the Bureau of Labor Statistics (BLS) for each year from 2011-2021. Projections for 2022-2023 were calculated using the average annual growth rate of 2.4 percent projected by the Centers for Medicare and Medicaid Services, Office of the Actuary for the period 2019-2028.
In years for which data was not yet available, disease prevalence was estimated using the average growth rate from the years in the past decade for which data was available, except for heart disease, for which growth was projected at 1 percent consistent with projections from the American Heart Association and with population growth.
Productivity costs to employers are based on prior estimates from Journal for Population Health Management. The per-person cost calculated for 2008 in that study was increased by the annual percentage change in the average employer cost of compensation, published by BLS, the same source used by JPHM. Total employer costs were calculated by multiplying the per-person cost by the prevalence estimate for 18 to 64 year-olds reduced by 5 percent to approximate the number of individuals with the disease not working.
Revenue loss estimates are equal to 20 percent of estimated lost wages. Lost wage estimates were calculated for both those not working at all due to chronic disease as well as estimates of reductions in wages for those working with a chronic disease. To estimate the reduction in the number employed, the analysis assumed a 5 percentage point increase in the labor force participation rate and then used the unemployment rate for each year to estimate the number of people who would otherwise be working if not for their chronic disease. For those working with a chronic disease, it assumed wages would otherwise be 7.5 percent higher (this is considered a conservative estimate as estimates from the literature reviewed ranged from 6 percent to 18 percent). Average annual wages were obtained from BLS. To forecast lost wages for 2021, 2022, and 2023, the analysis used the Employment Cost Index from Wells Fargo‘s latest economic forecast to estimate wage increases, and assumed the labor force participation rate for 2022 and 2023 would be 63 percent (the recent historical average leading up to the pandemic), that the unemployment rate would be 3.5 percent, and accounted for expected increases in the adult population. Overall disease prevalence was estimated at 41 percent among working-age adults (with obesity, heart disease, diabetes, and cancer being among the most common chronic diseases).
[i] https://data.worldbank.org/indicator/NY.GDP.MKTP.CD?locations=US
[ii] https://www.who.int/management/programme/ncd/Chronic-disease-an-economic-perspective.pdf
[iii] https://pubmed.ncbi.nlm.nih.gov/19339899/
[iv] https://www.cdc.gov/chronicdisease/resources/publications/factsheets/nutrition.htm, https://www.cdc.gov/media/releases/2017/p1003-vs-cancer-obesity.html
[v] https://www.nber.org/digest/nov07/why-developed-world-obese, https://www.cdc.gov/obesity/data/adult.html, https://www.census.gov/library/stories/2021/08/united-states-adult-population-grew-faster-than-nations-total-population-from-2010-to-2020.html
[vi] https://www.ahajournals.org/doi/10.1161/CIR.0000000000000950
[vii] https://www.cdc.gov/diabetes/basics/type2.html
[viii] https://seer.cancer.gov/statfacts/html/all.html
[ix] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6003578/
[x] https://pubmed.ncbi.nlm.nih.gov/29634829/#&gid=article-figures&pid=figure-2-uid-1
[xi] https://milkeninstitute.org/sites/default/files/reports-pdf/ChronicDiseases-HighRes-FINAL.pdf
[xii] https://www.kff.org/report-section/ehbs-2021-summary-of-findings/
[xiii] https://www.americanactionforum.org/research/background-understanding-the-connections-between-chronic-disease-and-individual-level-risk-factors/
[xiv] https://www.macpac.gov/wp-content/uploads/2021/12/MACStats-Medicaid-and-CHIP-Data-Book-December-2021.pdf
[xv] https://ideas.repec.org/a/eee/quaeco/v44y2004i1p102-121.html, http://www.healthaffairs.org/do/10.1377/hblog20160418.054518/full/
[xvi] https://ideas.repec.org/a/eee/quaeco/v44y2004i1p102-121.html
[xvii] https://www.schwabmoneywise.com/essentials/benefits-of-compound-growth
[xviii] https://www.sciencedirect.com/science/article/abs/pii/S0277953611006460
[xix] https://onlinelibrary.wiley.com/doi/full/10.1038/oby.2006.188, https://www.bls.gov/charts/employment-situation/civilian-labor-force-participation-rate.htm, https://data.bls.gov/pdq/SurveyOutputServlet
[xx] To the extent that employer costs are passed onto workers, there is the potential that those costs have been double-counted in this estimate.
[xxi] https://www.ibiweb.org/resource/cost-of-poor-health-infographic-2019-data/#gf_1
[xxii] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3128441/figure/f1/
[xxiii] http://pressbooks-dev.oer.hawaii.edu/humannutrition/chapter/the-endocrine-system/
[xxiv] https://www.ssa.gov/policy/docs/statcomps/di_asr/2015/sect01c.html#table24, https://www.ssa.gov/oact/STATS/dibGraphs.html#3
[xxv] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4580337/
[xxvi] https://www.fns.usda.gov/snap/eligibility/elderly-disabled-special-rules
[xxvii] https://www.fns.usda.gov/data/september-2021-keydata-report
[xxviii] https://www.cdc.gov/chronicdisease/resources/publications/factsheets/nutrition.htm