Weekly Checkup
May 8, 2020
Questions Around a COVID-19 Testing Regime
Policymakers are caught between two competing concerns. On the one hand, both infection rates and deaths from the coronavirus continue to climb in parts of the country. On the other, the nation’s economy has been decimated, and states are seeking to restart their economies as the economic pain mounts. Crucial to both fighting the pandemic and reopening sustainably will be a nationwide COVID-19 testing regime. But such a program raises myriad questions.
First, how should all the testing be tracked? Do we need a nationwide database of test results? What about privacy concerns? Additionally, not all tests are equal, as they vary in accuracy. Since different tests are not perfect substitutes, how should a database of testing results account for differences in test capability? Should only tests of a certain accuracy make the cutoff? Or should “inferior” tests be included but somehow weighted differently in any analysis? It is also important to keep in mind that in addition to testing for the virus, there are also serological tests that can document antibodies, and possible immunity, in those previously infected. How will these tests factor into a national testing regime?
Beyond the structuring of such a program lies a large set of questions around funding. Who should be paying for all this testing? Since copays and deductibles have been waived for COVID-19 testing thus far, insurers have been left holding the bag. But as testing scales up, who pays should ultimately depend on the reason the testing is being conducted. For example, an obvious reason for widespread testing revolves around public health considerations. The need to monitor for new or renewed outbreaks and to target future lockdowns and other social distancing measures effectively means there is an incentive for taxpayers to foot the bill for randomized infection testing with deidentified results. Does the benefit to the public here sufficiently merit public financing?
Another reason to test is to ensure the uninterrupted continuation of necessary services. First responders in the health and safety fields obviously need access to regular testing, but there are also workers in other fields, including those related to the nation’s supply chain, that should also receive testing. Postal employees, air crews, and those involved in freight rail and trucking provide critical benefit to the public. In addition to testing for infection, serological testing likely makes sense for this population. Do the benefits to the public of testing these essential personnel merit public financing?
Additionally, testing workers will likely become a standard cost of doing business for most employers for at least the next year or so. The need to provide a safe work environment and to minimize productivity losses from an outbreak among employees will compel employers to provide robust infection and antibody testing. Is it not reasonable to expect businesses to cover the cost here? Companies that don’t test will be at a competitive disadvantage compared with those who do. Should the cost of providing a safe work environment fall on taxpayers, rather than private enterprise?
Of course, some people will simply want to get tested. Under circumstances where testing has not been deemed medically necessary, people should be free to procure testing for infection or antibodies. But who pays for these tests? It seems right that those pursuing testing for their own information or peace of mind should pay for those costs themselves.
Adequate testing—both for current infections as well as serological testing for antibodies—is only one part of the three-legged stool on which any plan for moving the country forward amid the pandemic will rest. New treatments for COVID-19 patients as well as continued vaccine development will also be necessary, as AAF’s Andrew Strohman discusses here and here. But policymakers need to begin answering questions about how, who, and when to test, along with how to handle testing data, and who should be paying.
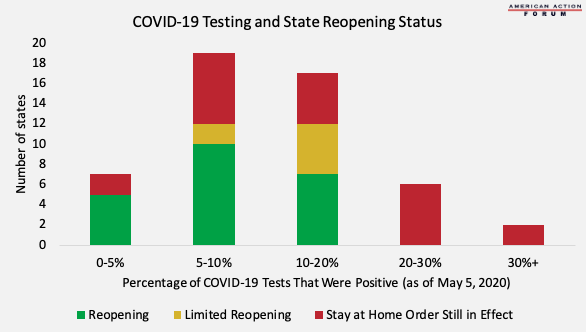
Chart Review: COVID-19 Testing and State Reopenings
Margaret Barnhorst, Heath Care Policy Intern
Across America, states and businesses are beginning to reopen after several weeks of government-mandated stay-at-home orders. Widespread testing is key to reopening the economy safely, and the United States is working to increase national testing capabilities, although more than half of the states are already testing enough people to put their positive COVID-19 rate at less than 10 percent of total tests. According to the World Health Organization, this benchmark (10 percent of positive tests out of total tests) indicates adequate testing in the community. States that choose to reopen with greater than 10 percent of COVID-19 tests coming back positive (currently 12 are doing so) will be particularly at risk for future outbreaks. Even if a state is currently showing a low percentage of positive tests, however, infections could still surge in areas where testing is inadequate. Looking ahead, Admiral Brett Giroir, a member of President Trump’s coronavirus task force, indicated that the United States is prioritizing increased testing for vulnerable and underserved populations.
Reopening statuses from The Chamber of Commerce and COVID-19 testing data from The Atlantic’s COVID-19 Tracking Project
Worth a Look
Wall Street Journal: Some Insurers Flex Balance Sheets to Help Hospitals, Doctors Amid Pandemic
Kaiser Health News: Eerie Emptiness of ERs Worries Doctors as Heart Attack and Stroke Patients Delay Care