Weekly Checkup
March 8, 2024
State of the U.S. Health Care System
Last night President Biden delivered his State of the Union Address and, as expected, touched on several health policy issues including drug pricing, insurance coverage, and Medicare. Beyond highlighting past actions by his administration, the president proposed several new initiatives. Let’s review the major new proposals and their potential effects on the health care system.
On drug pricing, the president proposed negotiating at least 50 drugs per year, rather than just the current 20 drugs under the negotiation scheme in the Inflation Reduction Act (IRA). The president also wants to expand the IRA’s $2,000 cap on Medicare Part D out-of-pocket costs to the private market, as well as cap monthly insulin costs for private patients at $35. Finally, the president pushed for Congress to expand the IRA’s Medicare inflation rebate penalties to all commercial drug sales.
The American Action Forum has written many, many insights on the effects that drug price “negotiation” in Medicare will have on access and innovation. We are already seeing the fallout, as drugs are getting pulled from development at a much higher rate than previously predicted. Expanding the number of drugs that will be negotiated is only going to make that problem worse. As for expanding the out-of-pocket cap in Part D to private insurance, such a move is likely to increase premiums for beneficiaries, just as they are projected to in Part D. The $35 cap on monthly insulin costs for private patients has been rendered almost moot by pharmaceutical manufacturers, who have already decided to limit monthly insulin costs to $35. The inflation penalty rebate will also cause drug prices to increase, as drug manufacturers will simply introduce drugs at higher prices to avoid the penalty.
On insurance coverage, President Biden called to make permanent of the temporary enhanced premium tax credits, which are set to expire at the end of this year, for Affordable Care Act (ACA) plans. Additionally, while he did not directly mention this in his address, in his pre-speech release the president called for extending surprise billing rules to ground ambulances and pushed for a final rule to make association health plans (AHPs) harder to access.
Making permanent the enhanced ACA subsidies, which were supposed to be temporary during the pandemic, is an extremely expensive proposal (the last extension cost an estimated $210 billion) with no proposed pay-for. Additionally, President Biden’s constant attacks on AHPs are likely to reduce options for quality, employer-sponsored insurance. By increasing subsidies and reducing private coverage options, these policies would likely increase dependency on government subsidies, bringing the U.S. health care system closer to a single-payer system.
Additionally, in his pre-address release, President Biden continued his demands that Congress provide “Medicaid-like coverage” to individuals in the 10 non-expansion states. He also proposed continuous insurance coverage for children from birth through age six, and that families should only be required to submit paperwork to prove eligibility for Medicaid every three years.
Here, we run into the issue that states, for which Medicaid represents the highest cost in their annual budgets, will see expenses increase significantly if they must guarantee lengthy coverage periods for children or families that may no longer need Medicaid coverage. This was an issue that states had to deal with during the pandemic-era freeze on Medicaid redeterminations, and the president’s proposal functionally continues that policy. Additionally, the “Medicaid-like coverage” proposal is likely to be extremely expensive for the federal government. Nowhere in the president’s proposals for enhanced Medicaid coverage was there mention of how to pay for them.
Regarding Medicare, the president asked Congress in his pre-speech press release to increase Medicare payroll taxes on high-income individuals, direct revenue from the net investment income tax into the Hospital Insurance trust fund, and use savings from drug price negotiation to bolster the trust fund. Additionally, the president objected to any attempts to reform Medicare benefits.
The president’s plan to hike payroll taxes on wealthy individuals wouldn’t come close to fixing the massive holes in Medicare’s solvency. Moreover, his pledge to not even consider reforms to benefits — a promise regrettably echoed by a bipartisan coalition of lawmakers – appears to have taken serious Medicare reform off the table. With Medicare’s 2031 bankruptcy fast approaching, it’s a particularly troubling time to limit our options to save one of America’s biggest entitlements.
In short, President Biden’s new proposals are expensive and ill-conceived. They are likely to have significant negative externalities across the health care system by increasing the debt, reducing access to new drugs, increasing drug prices, draining state budgets, raising premiums, and reducing access to new insurance options. So, what’s the state of the U.S. health care system? It looks worse-off than ever.
Chart Review: Underlying Causes of Pregnancy-related Deaths
Anna Grace Shepherd, Health Policy Intern
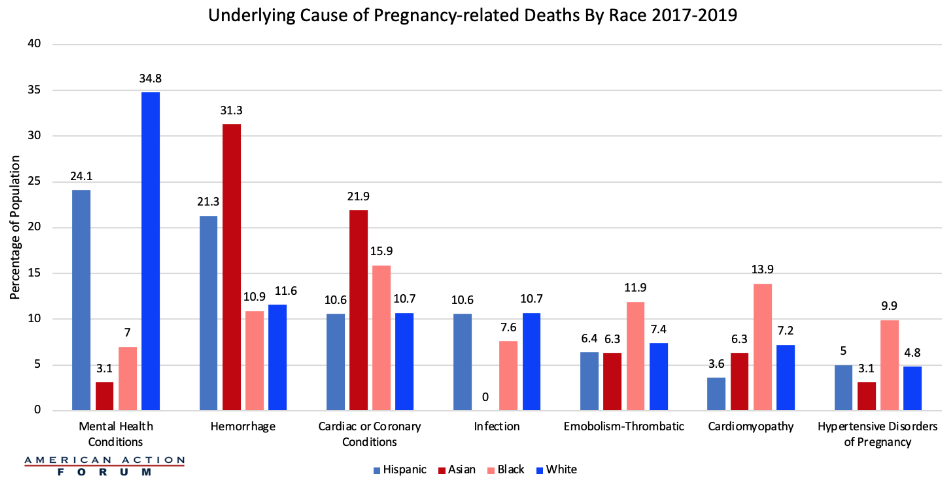
In 2019, the United States maternal mortality rate was 20.1 deaths per 100,000 live births but has since risen to 23.8 deaths per 100,000 live births in 2020 and to 32.9 deaths per 100,000 live births in 2021. As reviewed in the chart below, a study conducted by Maternal Mortality Review Committees in 36 states broke down by race the underlying cause of pregnancy-associated deaths between 2017 and 2019. Among the 987 deaths recorded in the study, the seven most frequent causes of pregnancy-related deaths were mental health conditions, hemorrhage, cardiac and coronary conditions, infection, thrombotic embolism, cardiomyopathy, and pregnancy-related hypertension. These seven conditions accounted for over 80 percent of pregnancy-related deaths within the study.
As the chart below demonstrates, underlying causes of pregnancy-related deaths varied by race and ethnicity. Mental health conditions, including suicide and overdoses, were the leading cause of pregnancy-related deaths for both Hispanic and non-Hispanic White women. For non-Hispanic Black women, cardiac and coronary conditions were the leading cause of death, and non-Hispanic Black women were more likely to die from thrombotic embolisms, cardiomyopathy, or pregnancy-related hypertension than any other race or ethnicity. For non-Hispanic Asian women, hemorrhages were the leading cause of death, with this same population of post-partum women being the most likely to die from hemorrhages than any other race or ethnicity.
These demographic differences in cause of death point to the need to provide tailored services and therapies to postpartum women depending on the types of diseases and conditions to which they may be more susceptible. What’s more, with the rate of maternal mortality rising, policymakers should consider ways to incentivize assessments of clinical risks and outcomes to help new mothers.
Source: Pregnancy-Related Deaths: Data from Maternal Mortality Review Committees in 36 US States, 2017–2019