Weekly Checkup
April 30, 2021
What Happened to Biden’s Health Care Agenda?
This week President Biden addressed a joint session of Congress, laying out his American Families Plan (AFP). Biden campaigned on a public health insurance option, lowering the Medicare eligibility age, and cutting prescription drug prices, but in what was expected to be his big health care package, all were absent. Biden punted on a host of health policy priorities that progressives are clamoring for, even as he paid lip service to them.
When Biden signed the American Rescue Plan (ARP) in March, it was seen as a down payment on Biden’s health policy agenda. The legislation contained several substantial health initiatives and lots of health spending, but top progressive objectives were left out. Health policy was then expected to move in the second package, the broadly defined infrastructure package. That package, which is still embryonic, has since been split in two. Health care, except for a large investment in home based long-term care, was squeezed out of American Jobs Plan and pushed to the AFP. Many congressional progressives were expecting Biden to use their extreme drug pricing legislation, H.R. 3, as a revenue source in the AFP, but it wasn’t to be. The AFP largely steers clear of health policy, focusing on tax changes, childcare, education, and paid leave. The one significant health policy—and it is significant, to be fair—is a permanent extension of changes the ARP made to the Affordable Care Act’s (ACA) health insurance subsidy framework.
Effectively what this means is that the ARP really was the high-water mark for Biden’s health care push this year. To say the least, this is surprising. Biden did call on Congress to take action this year on various health policy priorities—drug prices in particular—but just not as part of any of the reconciliation bills Democrats hope to pass. The challenges to passing other legislation, especially for H.R. 3, are twofold.
First, there’s the congressional calendar. If the American Jobs Plan is done using reconciliation—necessary to avoid a filibuster in the Senate—then Congress will first have to try a never before used maneuver and amend the 2021 Budget Resolution and create a new set of reconciliation instructions. This won’t be a full budget process, but it will require both the House and Senate to debate and pass a budget amendment, including a lengthy amendment process in the Senate before work can start on the reconciliation bill. Once the House passes the AJP, it will have to be reviewed by the Senate parliamentarian to determine if any provisions violate reconciliation rules. If the Senate tries to simultaneously move a bipartisan infrastructure bill, you can tack on even more floor time. Then Congress will have to pass a 2022 Budget Resolution to get a third set of reconciliation instructions, rinse repeat. At the same time Congress will have to fund the government before the end of September and likely increase the debt limit. In other words, it’s not entirely clear that Congress will be able to even pass the AFP before the end of the year, much less a stand-alone bill on drug prices or lowering the Medicare age.
The second issue, of course, is that H.R. 3 can’t avoid a Senate filibuster, so if it’s not part of a reconciliation package, it’s dead on arrival in the Senate, even if House Democrats can pull together enough votes to pass it. It’s possible, even likely, that some congressional Democrats will try to include the provisions of H.R. 3 in the AFP reconciliation package anyway, but by leaving it out of his proposal, Biden has given cover to more moderate members in the House and Senate who may be uncomfortable with H.R. 3’s extreme policies to reject the effort. Progressive hopes to dictate drug prices, lower the Medicare age, and implement a public option can’t pass outside of reconciliation—and in the case of the latter two may not qualify for reconciliation—and Biden just made it much harder to include any of them in reconciliation.
The upshot of all this is that the ACA subsidy enhancements—temporary in the ARP and permanent if the AFP becomes law—along with the proposed expansion of home health care could end up being the sum of Biden’s health policy agenda this year, surely disappointing many on the left.
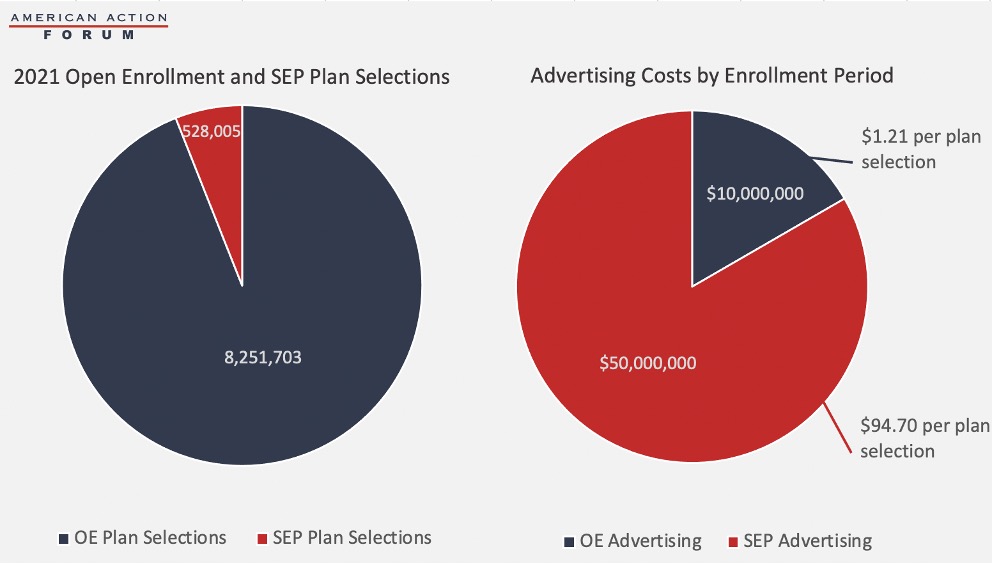
Chart Review: Advertising Costs for the ACA Special Enrollment Period
Madeline VanHorn, Health Care and Human Welfare Policy Intern
The Biden Administration authorized a Special Enrollment Period (SEP) in response to the pandemic, beginning February 15 and set to continue until August 15. Health and Human Services (HHS) and the Centers for Medicare and Medicaid Services (CMS) have launched advertising campaigns to raise awareness of the SEP, including digital and broadcast advertising as well as email and text communications. In January before the SEP began, CMS committed $50 million to advertising. Another $50 million for the educational campaign was announced on April 15, meaning the total funding for these campaigns is $100 million. In the period from February 15 to March 15, 528,000 plan selections were made—compared to 209,000 plan selections in 2020 when there was no blanket SEP and instead people could only enroll through an SEP as their circumstances permitted. Considering the amount spent on advertising, this enrollment comes to almost $95 dollars per plan selection. Below this sum is compared to the amount spent on advertising during open enrollment, $10 million. For comparison, during open enrollment for the 2021 plan year the United States saw over 8.2 million plan selections, and advertising cost per plan selection was $1.21.
Source: Centers for Medicare and Medicaid Services
Tracking COVID-19 Cases and Vaccinations
Christopher Holt, Director of Health Care Policy
To track the progress in vaccinations, the Weekly Checkup will compile the most relevant statistics for the week, with the seven-day period ending on the Wednesday of each week.
| Week Ending: | New COVID-19 Cases: 7-day average |
Newly Fully Vaccinated: 7-Day Average |
Daily Deaths: 7-Day Average |
|
April 28, 2021 |
52,528 |
1,048,901 |
628 |
|
April 21, 2021 |
62,652 |
1,409,539 |
684 |
|
April 14, 2021 |
69,625 |
1,666,483 |
714 |
|
April 7, 2021 |
64,387 |
1,511,655 |
637 |
|
March 31, 2021 |
63,484 |
1,320,636 |
825 |
|
March 24, 2021 |
57,213 |
936,035 |
857 |
|
March 17, 2021 |
53,062 |
998,497 |
946 |
|
March 10, 2021 |
54,980 |
933,776 |
1,355 |
|
March 3, 2021 |
62,407 |
893,243 |
1,648 |
|
Feb. 24, 2021 |
66,328 |
827,235 |
1,984 |
|
Feb. 17, 2021 |
76,419 |
730,475 |
2,081 |
|
Feb. 10, 2021 |
103,089 |
686,634 |
2,652 |
|
Feb. 3, 2021 |
133,804 |
472,857 |
2,880 |
|
Jan. 27, 2021 |
161,210 |
328,880 |
3,229 |
Sources: Centers for Disease Control and Prevention Trends in COVID-19 Cases and Deaths in the US, and Trends in COVID-19 Vaccinations in the US
Note: The U.S. population is 330,233,976.
Worth a Look
The Hill: Democrats push to add drug pricing, Medicare measures to Biden plan
New York Times: How Pfizer Makes Its Covid-19 Vaccine